For CY 2020, CMS is increasing payment for transitional care management (TCM) services which are care management services provided to beneficiaries after discharge from an inpatient stay or certain outpatient stays.
Payments to practitioners will increase for the transitional care they provide as patients move from the hospital to follow-up care, which is important for patients because it ensures the continuity of their care. Improvements will also be made to chronic care management services for patients with multiple chronic conditions. In addition to the existing payments for chronic care management services, practitioners can be paid more if they spend more time on these care management services. Patients with chronic care needs who use the healthcare system more frequently benefit from this additional care coordination.”
Chronic Care Management Reimbursement for Single, High-Risk Patients
CMS is creating a Medicare-specific code for additional time spent beyond the initial 20 minutes allowed in the current coding for chronic care management (CCM) services, which are services provided to beneficiaries with multiple chronic conditions over a calendar month.
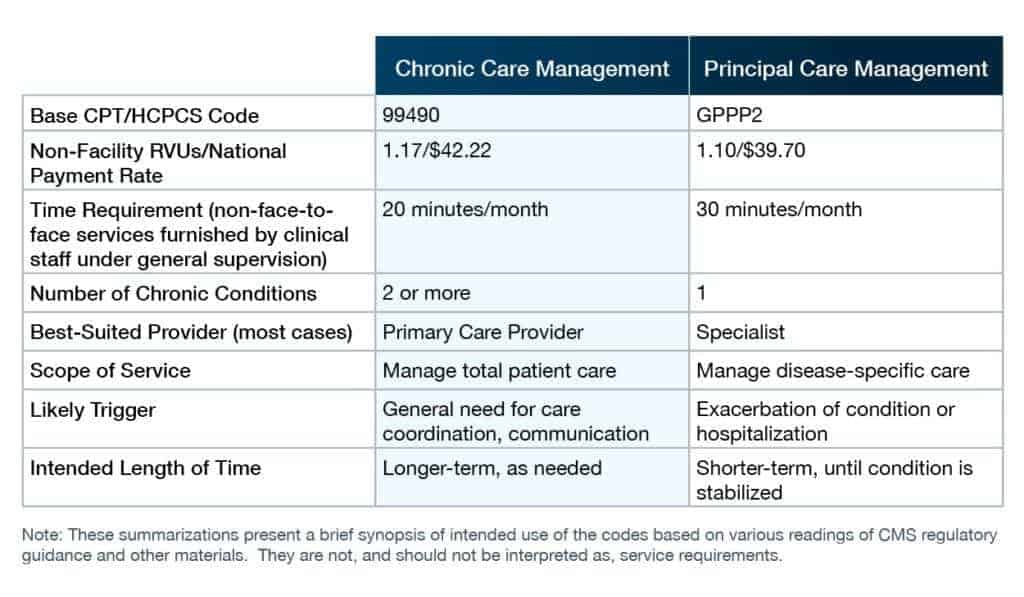
Currently, Chronic Care Management (CCM) is only applicable to beneficiaries with more than one complex condition. Recognizing that beneficiaries with only one complex condition can also benefit from CCM services, CMS introduces, Principal Care Management (PCM) to address ongoing management of beneficiaries with one complex condition.
The Principal Care Management (PCM) code separately pays for care management of patients with single, high-risk chronic condition such as diabetes or high blood pressure, ensuring that patients with one high risk condition can receive important care management services such as checking medication adherence and coordinating care.
Here’s an example:
CMS now proposes to reimburse physicians for principal care management (PCM) furnished to beneficiaries with a single chronic condition. CMS contemplates that PCM services will be furnished under the supervision of a specialist for a limited time to stabilize the beneficiary’s condition. The following summarizes the key differences between CCM and PCM services:

Lisa Remington is president and publisher of the Remington Report magazine and President of Remington’s Home Care Leadership Think Tank. She has worked with more than 10,000 organizations in both a consultancy role and an educator. Lisa monitors the complex key trends and forces of change to develop a correct strategic approach to de-risk decision-making and create sustainable futures across the healthcare continuum.
