Evolving care delivery models such as ACOs, Bundled Payments, and Hospital-at-Home programs has led to a vital shift toward team-based approaches. These models emphasize collaboration and leveraging diverse expertise to provide comprehensive and effective patient care. This shift is largely driven by workforce shortages, clinician burnout, and the focus on patient-centered care.
In a team-based approach, members come together as a whole to discuss their individual assessments and develop a joint service plan for the patient. Practitioners may blur some disciplinary boundaries but still maintain a discipline-specific base (for instance, aspects of functional assessments may be shared across disciplines). Teams integrate closer to complete a shared goal. (Ellis & Sevdalis, 2019).
Hospice Team-Based Care
An example of a team-based approach is in hospice. Hospice team-based care is an approach where a multidisciplinary team of healthcare professionals works together to provide comprehensive care to patients who are in the final stages of a terminal illness. The goal of hospice care is to ensure that patients experience a high quality of life during their remaining time, focusing on comfort, dignity, and symptom management rather than curative treatment.
Key Components of Hospice Team-Based Care
- Multidisciplinary Team: The hospice care team typically includes doctors, nurses, social workers, chaplains, home health aides, and volunteers. Each member plays a specific role in addressing the physical, emotional, social, and spiritual needs of the patient and their family.
- Patient-Centered Care: Care is tailored to the individual needs and wishes of the patient. The team works closely with the patient and their family to develop a personalized care plan that reflects the patient’s values and preferences.
- Pain and Symptom Management: One of the primary focuses of hospice care is to manage pain and other distressing symptoms such as nausea, shortness of breath, and anxiety. This is achieved through medication, therapies, and support from the care team.
- Emotional and Spiritual Support: The hospice team provides emotional support to both the patient and their family, helping them cope with the psychological aspects of terminal illness. Spiritual care is also available for those who seek it, often provided by chaplains or spiritual advisors.
- Family Involvement: Families are an integral part of the hospice care process. The team provides education, support, and respite care to help families manage their loved one’s care and their own emotional needs.
- Coordination of Care: The hospice team coordinates care across various settings, whether at home, in a hospice facility, or in a hospital. This ensures continuity of care and that the patient’s needs are met regardless of where they are receiving care.
- Bereavement Support: After the patient’s death, hospice care continues to support the family through bereavement services, helping them process their grief and adjust to life without their loved one.
This team-based approach in hospice care ensures that the patient receives holistic care, addressing not just the physical symptoms but also the emotional, social, and spiritual aspects of end-of-life care. The collaboration among different professionals allows for comprehensive and compassionate care tailored to the needs of both the patient and their family
Another example of team-based care occurs within the four walls of hospitals. It’s crucial to note that hospitals are reevaluating their nurse-to-patient ratios model. Instead of assigning one nurse to oversee a small group of patients to one RN, a team-based approach of several staff members work at the top of their license to care for a larger group of patients.
2 Different Approaches to Team-based Care
Though often used interchangeably, multidisciplinary and interdisciplinary differ in their form and function.
Multidisciplinary Care Teams: A team composed of members from more than one discipline, offering patients a greater breadth of services. Team members work independently and in parallel, with each provider responsible for his or her own area. Communication between team members is formal, and team structure is often hierarchical with a designated leader overseeing the team.
Interdisciplinary Care Teams: A team of professionals from various disciplines is involved in reaching a common goal, with each team member bringing his or her discipline’s expertise to the team. Team members work formally and informally, and information is shared in a systemic way among team members. An interdisciplinary team is collaborative and integrates each profession’s knowledge into the care plan.1
5 Core Principles for Fostering Effective Teams
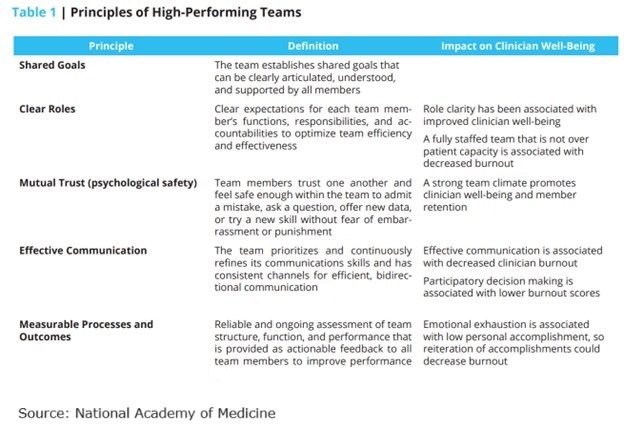
The National Academy of Medicine identified five core principles to enable care providers to foster effective care teams. Those principles are:
Shared Goals. The team establishes shared goals that reflect the priorities of the patient and family. The goals are clearly articulated, understood, and supported by all team members.
Clear Roles. There are clear expectations for each team member’s functions, responsibilities, and accountabilities.
Mutual Trust. Team members trust one another and feel safe to admit a mistake, ask a question, offer new data, or try a new skill without fear of embarrassment or punishment.
Effective Communication. The team prioritizes and continuously refines its communications skills and has consistent channels for efficient, bidirectional communication.
Mutual Processes and Outcomes. A reliable and ongoing assessment of team structure, function, and performance is provided as actionable feedback to all team members to improve performance.
How Team-based Reduces Clinician Burnout
As workforce challenges persist, team-based care not only addresses the shortage of healthcare workers but also has the potential to significantly improve patient outcomes by enhancing quality and safety. This approach can increase productivity and boost job satisfaction by reducing individual workloads and preventing burnout.
High-functioning clinical teams are essential for the delivery of high-value healthcare and have been associated with:
- Decreased workloads
- Increased efficiency
- Improved quality of care
- Improved patient outcomes
- Decreased clinician burnout/turnover
Table 1 describes the Principles of High-Performing Teams and the relationships between team-based care and the impact of improving clinician burnout.
4 Characteristics of Successful Teamwork
A team-based model of care strives to meet patient needs and preferences by actively engaging patients as full participants in their care while encouraging all healthcare professionals to function to the full extent of their education, certification, and experience. 2
Successful teamwork has four key characteristics:
- a clear and compelling purpose or goal,
- an enabling social structure that facilitates teamwork,
- a supportive organizational context, and
- expert teamwork coaching.3
Effective teamwork depends on:
- the team member’s psychological safety, defined as their ability to trust one another and feel safe enough within the team to admit a mistake, ask a question, offer new data, or try a new skill without fear of embarrassment or punishment; and
- allows team members to learn, teach, communicate, reason, think together, and achieve shared goals, irrespective of their individual positions or status outside the team.4
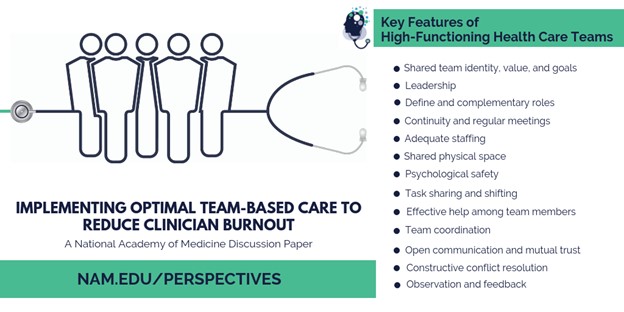
Team-based health care has been linked to improved patient outcomes and may also be a means to improve clinician well-being. 5 The increasingly fragmented and complex healthcare landscape adds urgency to the need to foster effective team-based care to improve both the patient’s and team’s experience of care delivery.
Resources
- columbia.edu/projects/sl2/pdf/glossary.pdf.
- American College of Obstetricians and Gynecologists. 2016. Collaboration in practice: Implementing team based care.
- Gordon, S., D. L. Feldman, and M. Leonard. 2014. Collaborative caring: Stories and reflections on teamwork in health care.
- Hackman, R. 2014. What makes for a great team?Washington, DC: American Psychological Association
- Welp, A., and T. Manser. 2016. Integrating teamwork, clinician occupational well-being, and patient safety – development of a conceptual framework based on a systematic review.

Lisa is a turnaround expert who excels in navigating unsteady, complex, and ambiguous environments. She has provided C-suite education to over 10,000 organizations in the home care sector for decades. Lisa’s trusted voice in the industry has been recognized for her ability to manage disruption, identify new growth and revenue opportunities, and develop high-level engagement strategies between home care and referral partnerships. Her contributions are instrumental in advancing the future of home care.
Other Articles You Might Enjoy
Improving Outcomes Between Home Care and Medicare Advantage Plans
Home care services have emerged as a critical strategy for improving health outcomes, reducing hospital readmissions, addressing both clinical and non-clinical needs, and improved patient satisfaction among Medicare Advantage beneficiaries.
Average 30-Day Readmission Rates by Medical Conditions
We provide critical readmission data about average readmission rates, condition-specific readmission rates, and hospitals with high and low readmission rates.
Hospital-at-Home Readmissions: Which Medical Conditions Created the Highest and Lowest Readmissions?
CMS’s report on the Acute Hospital Care at Home (AHCAH) initiative highlighted the highest and lowest readmission rates by medical conditions.





