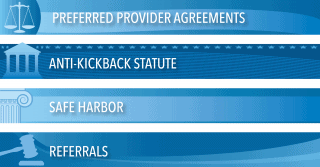
Legal: Recent Case Demonstrates Pitfalls of Getting Referrals from Assisted Living and Independent Living Facilities
In this article is the legal case between referrals: assisted living, independent living facilities, and home health, details of the ruling, and what to consider in a referral relationship agreement.