Tackling Alzheimer’s and Dementia Readmissions and ED Visits
May/June 2024 Issue
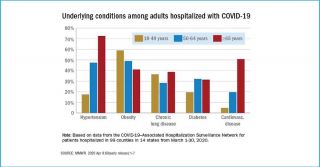
SUBSCRIBER CONTENT In 2024, approximately 2.4 million individuals with Alzheimer’s dementia are aged 85 or above. Research indicates that patients who receive home health services following hospital discharge have a higher chance of staying in their community for at least 30 days post-discharge, with more significant advantages observed with extended durations of home health care.