Most accountable care organizations (ACOs) report having comprehensive chronic care management processes or programs in place to manage people with complex needs.
An analysis from the National Survey if ACOs, explored several questions regarding the use of evidence-based approaches to managing the care of complex patients including risk stratification, segmentation, improvement in care transitions, engagement of patients and families in care decisions, and chronic condition management.
Given an ACOs incentive to reduce cost and improve quality, ACOs often employ care management programs that follow evidence-based strategies for increasing the value of care delivered to people with complex needs.
These strategies include:
- identifying people who are at high risk for adverse clinical events (often referred to as risk stratification)
- separating high-risk patients into subgroups with common needs (segmentation)
- improving care transitions across settings
- engaging individuals and their families in care decisions
- using programs that help patients address chronic illness.
Understanding the variation in ACOs’ use of these strategies is a useful first step in determining a standard of care for this population.
Key Findings
Most ACOs report having comprehensive chronic care management processes or programs in place to manage people with complex needs. More labor-intensive interventions, however, are rare. Few ACOs report having advanced programs for engaging patients, in-home visits after hospital discharge, or evidence-based services for patients needing mental health or addiction treatment.
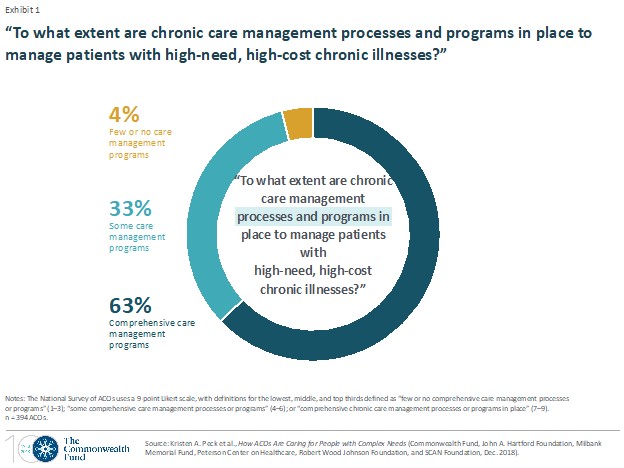
In the survey, most ACOs (63%) report having comprehensive care management programs and processes (referred to here as simply “care management programs”) in place, based on their response of 7 or higher on a 9-point scale (Exhibit 1). In contrast, 33 percent report they have only “some” care management programs in place, while 4 percent say they have “few or no” such programs.
Engaging and Activating Patients
Engaging and activating patients has been shown to decrease long-term health care costs and to improve health care experiences. Yet even among ACOs with comprehensive care management programs, clinician training in activation and engagement is limited, as are programs to encourage patient involvement in care decisions.
Only two of every five (38%) ACOs with comprehensive care management programs report that most or all their affiliated clinicians are trained in patient activation and engagement methods. And just 38 percent of these ACOs have advanced programs in place for clinicians to encourage ACO patients to be actively involved in decisions involving their care and in self-managing their conditions. The percentages are even lower for other ACOs, only 16 percent of which respond that most or all their clinicians are trained in patient engagement and 15 percent of which report having comprehensive programs to encourage patient involvement.
Care Transitions
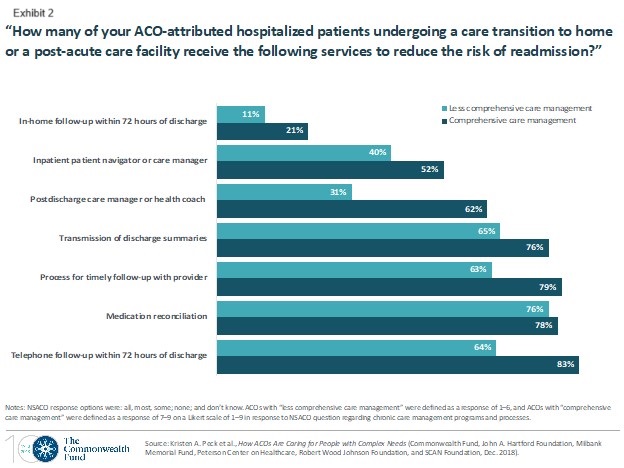
The National Survey of ACOs asked organizations about seven components of evidence-based interventions designed to reduce risk of readmission for hospitalized individuals who are transitioning to home or a post-acute care facility. ACOs reported use of interventions requiring one-on-one interaction between providers and patients is low.
Despite being a prominent component of evidence-based care transition models, in-home follow-up is the least commonly used strategy for patients undergoing a care transition. Only 21 percent of surveyed ACOs with comprehensive care management programs report that most or all patients receive an in-home follow-up visit within 72 hours of discharge. And only 11 percent of the remaining ACOs said that most or all patients receive this in-home visit. (Exhibit 2).
Other Articles You Might Enjoy
5 Ways High-Functioning Team-Based Care Reduces Clinician Burnout
Evolving care delivery models emphasize collaboration and leveraging diverse expertise to provide comprehensive and effective patient care. This shift is largely driven by workforce shortages, clinician burnout, and the focus on patient-centered care.
Best Practices for Effective Strategy Execution
Effective strategy execution is crucial for success, as even the most well-crafted strategies can fail if not properly implemented.
5 Reasons Why a 5-Year Strategic Plan May Pose Challenges
Five-year strategic plans in home care often encounter several challenges due to the dynamic nature of the industry.





