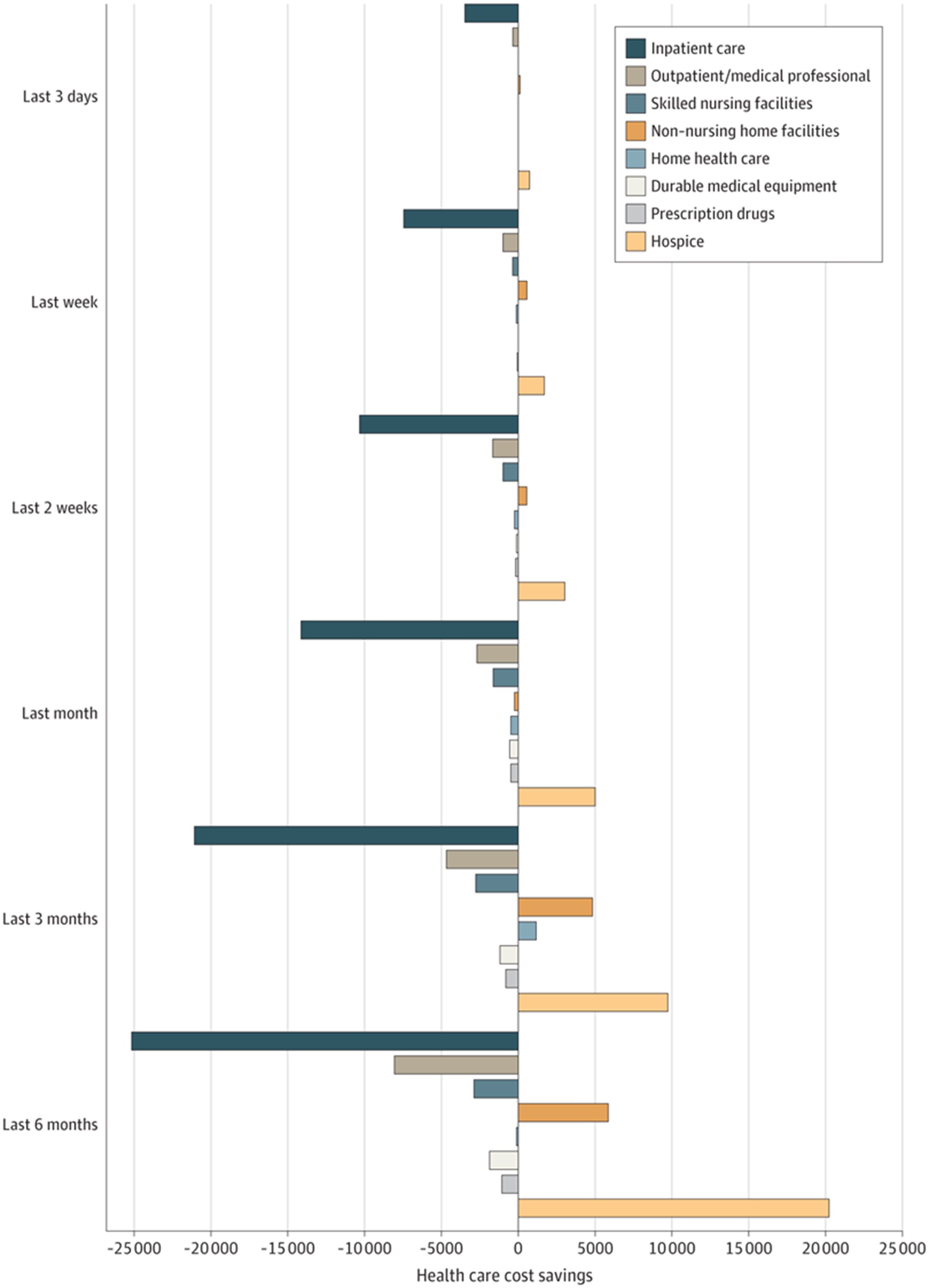
The breakdown of savings by days, weeks, and months
A recent study published in the Journal of the American Medical Association of 5,464 beneficiaries reveals that total health expenditures were lower for those who used hospice compared with propensity score-weighted non-hospice control participants for the:
- last 3 days of life ($2,813 lower)
- last week of life ($6,806 lower)
- last 2 weeks of life ($8,785 lower)
- last month of life ($11,747 lower)
- last 3 months of life ($10,908 lower)
The main outcomes and measures: Total health care expenditures were measured across payers (family out-of-pocket, Medicare, Medicare private health maintenance organizations, Veterans Administration, and other) and by expenditure type (inpatient care, outpatient care, medical visits, skilled nursing, home health, hospice, durable medical equipment, and prescription drugs).
Figure 1. Adjusted Health Care Cost Savings for Individuals Enrolled with Hospice Compared with Non-Hospice Control Participants by Health Care Event, 2002-2018
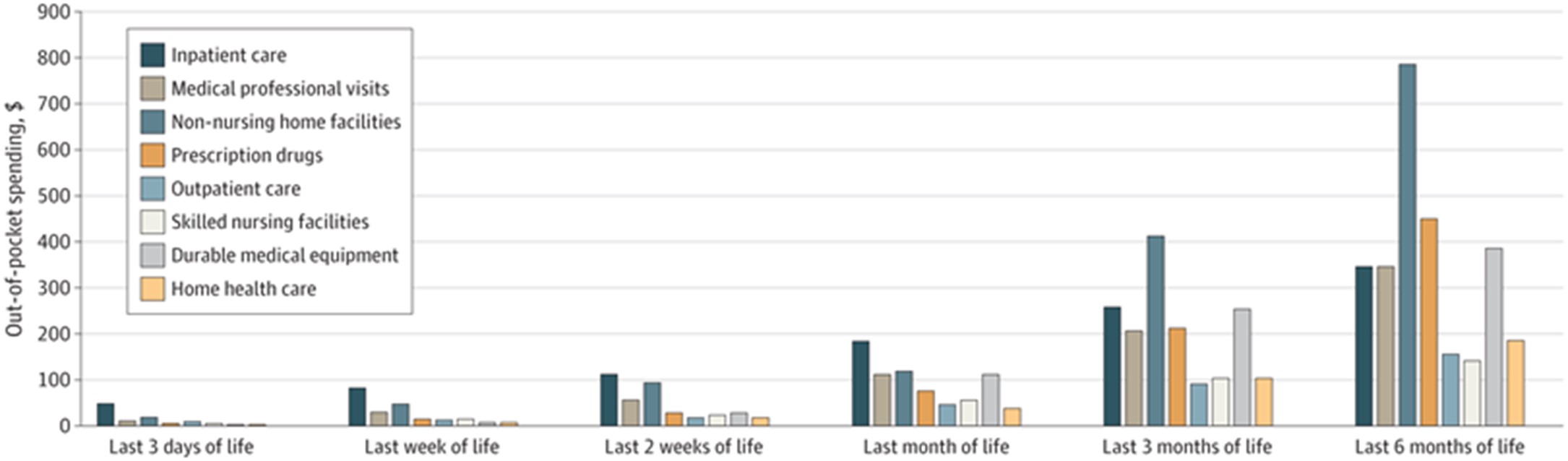
Family out-of-pocket expenditures were lower for hospice enrollees in the last three days of life ($71); last week of life ($216); last 2 weeks of life ($265); and last month of life ($670) compared with those who did not use hospice. (Figure 2)
Figure 2. Family Out-of-Pocket Health Care Expenditures of the Entire Study Population at the End of Life (N = 5464), 2002-2018
Private insurance expenditures were lower for those who enrolled with hospice compared with those who did not enroll with hospice for all periods examine. See Table 2.
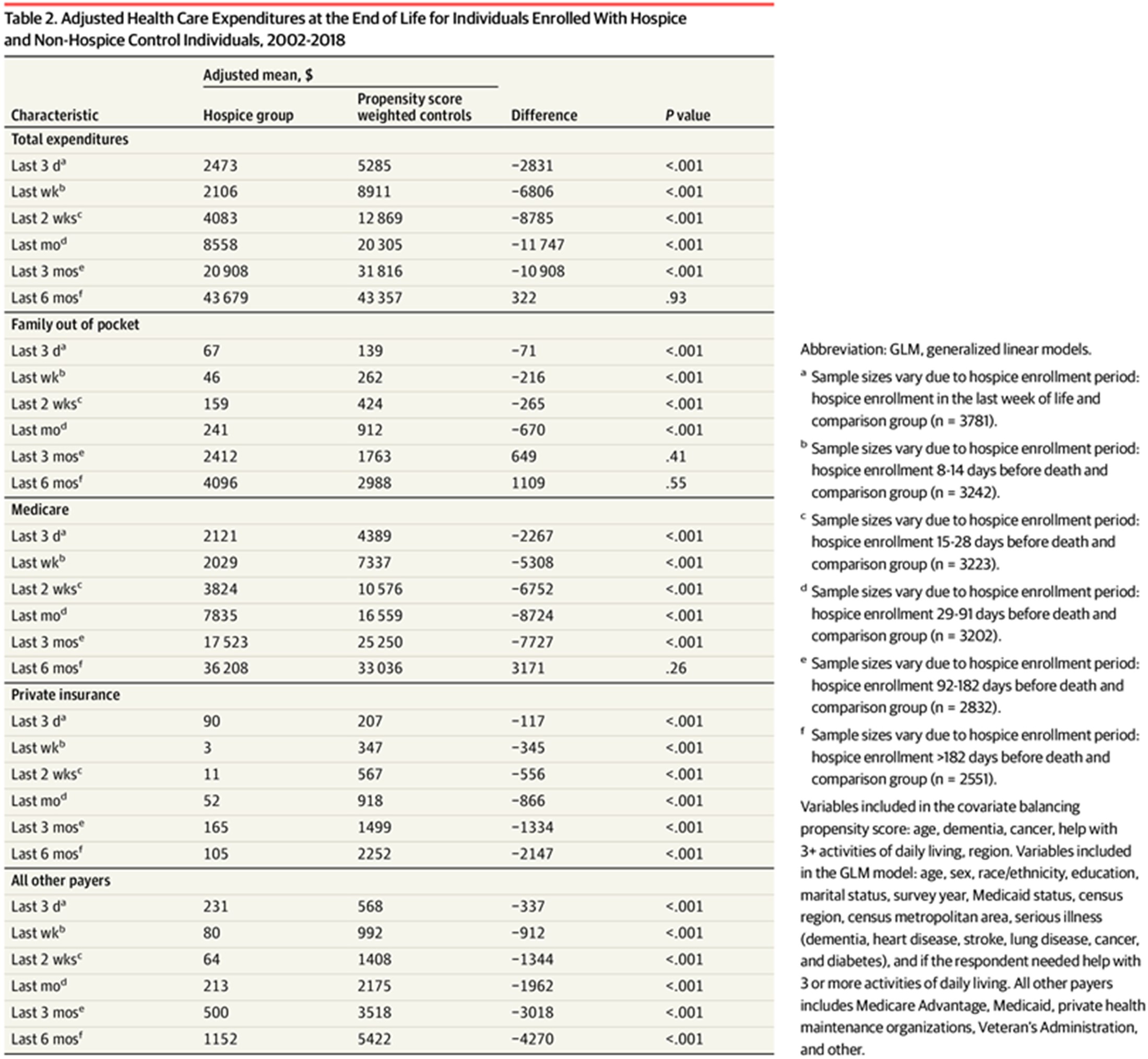
Hospice was associated with lower total health care expenditures across all payers and families primarily owing to lower spending for inpatient care. The study concluded that the findings of this cohort study suggest that hospice use is an example of a health care model that demonstrates both components of the value proposition: it improves the quality of end-of-life care and is associated with lower health care costs. Moreover, unlike many other aspects of our health care system, cost reductions to insurers in the present study did not translate into higher costs for patients and their families.
Other Articles You Might Enjoy
High-Need Patients: Utilization of Home Care
Finding ways to improve outcomes and reduce spending for patients with complex and costly care needs requires an understanding of their unique needs and characteristics.
5 Ways High-Functioning Team-Based Care Reduces Clinician Burnout
Evolving care delivery models emphasize collaboration and leveraging diverse expertise to provide comprehensive and effective patient care. This shift is largely driven by workforce shortages, clinician burnout, and the focus on patient-centered care.
ACOs: The Critical Role of Care Coordinators in Discharge Planning and Care Transitions
Lessons from 20 Medicare Shared Savings Programs provide insight into how ACOs manage complex care patients.





