Almost half of all people aged 45-64, and 80% of those 65 and over, have multiple chronic conditions. Finding ways to improve outcomes and reduce spending for patients with complex and costly care needs requires an understanding of their unique needs and characteristics.
The share of adults who have multiple chronic diseases as well as a limitation that hinders their ability to carry out necessary daily activities such as bathing, eating, using the telephone, or taking medication is much smaller than the share with multiple chronic diseases alone.
This information is useful to know:
- The number of home health days utilized on average by high need patients.
- The functional status of high need patients.
- Characteristics of high-need patients.
More Doctor’s Visits and Paid Home Health Care Days
High-need patients visited the doctor an average of 9.6 times a year, about 50% more on average than adults with multiple chronic conditions only and nearly three times as often as adults overall.
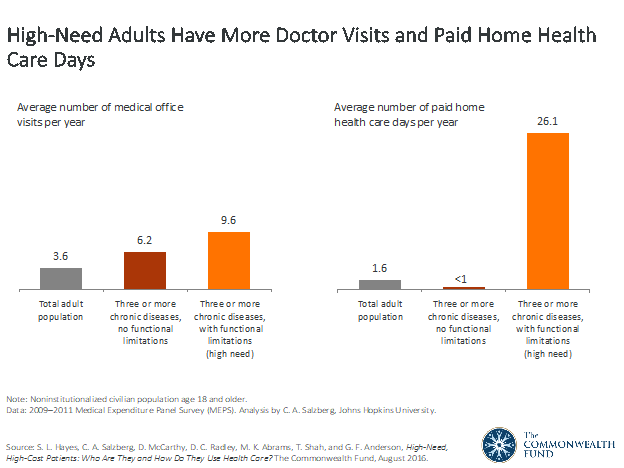
High-need adults used 26 paid home health care days on average over the course of a year compared to roughly one day per year among individuals with multiple chronic conditions only or the average U.S. adult population. The higher rate of use of paid home health care by high-need patients likely reflects their functional limitations, which may contribute to meeting criteria for coverage of such services by Medicare, Medicaid, or other payers, under certain circumstance.
High-Cost Patients Have Multiple Chronic Diseases, With or Without Functional Limitations
The high-need group exhibited variation in their use of services and in the demographics of those who utilized them. Only slightly more than a third (36%) made 10 or more visits to the doctor in a year, while a slightly greater share (43%) had five or fewer visits. Patients with a higher average number of doctor’s visits were under age 65, had relatively high income, were college-educated, and were privately insured. The opposite was true for paid home health care, with the highest use among the oldest (age 75 and older), the poorest, the least educated, and those dually eligible for Medicare and Medicaid. Paid home health care was concentrated among a fraction of patients: 12% used more than 60 days compared to nearly three-quarters who used no paid home health care days at.
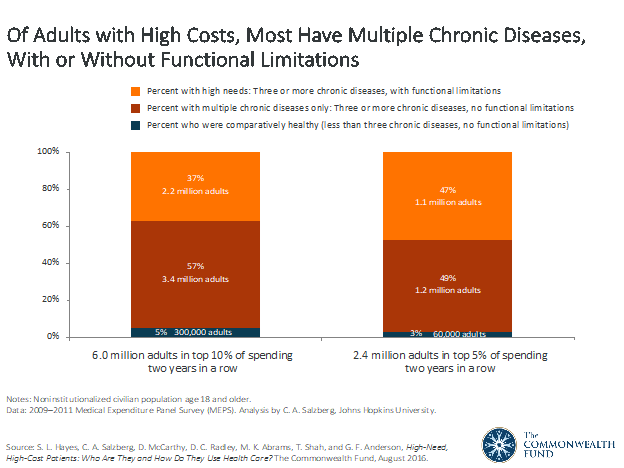
The total number of adults who incurred high health care spending for two years in a row were distributed based on their clinical complexity. Nearly all high spenders have multiple chronic diseases, either with or without functional limitations. As the top spending category narrowed, however, to 5% from 10%, the share of people within it who had a functional limitation in addition to multiple chronic diseases – that is, the group we identified as high-need adults – grew: they represented a little over a third (37%) of those in the top 10% of health spending in both years but almost half (47%) of those in the top 5% of spending.
The Greater the Need, the Higher the Spending
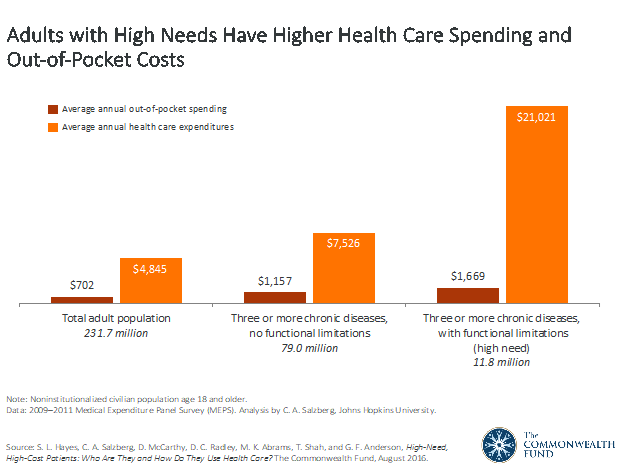
For high-need adults, average annual per-person spending on health care services and prescription medicines topped $21,000, nearly three times the average for adults with multiple chronic diseases only, and more than four times the average for all U.S. adult. High-need adults spent more than twice as much, on average, on out-of-pocket expenses as adults in the total population ($1,669 vs. $702, while their annual median household income was less than half that of the overall adult population ($25,668 vs. $52,685). In contrast, average out-of-pocket spending for patients with multiple chronic diseases and no functional limitations was about a third less ($1,157) than that of high-need adults ($1,669); their annual median income was about the same as adults in the overall population ($52,499).
Key Sociodemographic and Health Status Differences
Understanding how high-need adults differ from other adults can help health systems, payers, and hone care providers design and target programs.
High-need adults are disproportionately:
- Older: More than half were age 65 and older; of these, most were 75 and older. In contrast, only about a third of adults with multiple chronic diseases, and less than a fifth of the adult population as a whole, were age 65 and older.
- Female: Nearly two-thirds of adults with high needs were women, compared to just over half of the total population. This may reflect the fact that the majority of high-need adults are older and that women tend to live longer than men.
- White: Nearly three-quarters of adults with high needs were white non-Hispanic—a higher share than in the adult population as a whole. Hispanic and Asian adults were underrepresented in both the high need and the multiple chronic diseases–only groups.
- Less educated. More than one of four high-need adults did not finish high school, compared with one of seven of those with multiple chronic diseases and about one of six in the total adult population.
- Low income. More than half of adults with high needs had low incomes (i.e., below 200% of the federal poverty level, or less than $21,780 for an individual). This is nearly double the share in both the multiple chronic conditions-only group and the total adult population.
- Publicly insured. Nearly all adults with high needs had health insurance – only 4% were uninsured at the time of the survey, which was fielded before the Affordable Care Act’s major coverage expansions. More than four of five adults with high needs were covered by public insurance: Medicare, Medicaid, or a combination of the two, reflecting their older age and lower incomes. In contrast, only about two of five adults with multiple chronic conditions only, and even less in the total adult population, were covered by public insurance.
- Fair or poor self-reported health. The combination of a functional limitation and multiple chronic conditions appears to lead to worse self-reported health than multiple chronic conditions alone. While more than four of five adults with high needs (83%) reported fair or poor health, fewer than two of five adults (38%) in the multiple chronic diseases–only group did so.
It is important to consider the unique needs of the subpopulation with functional limitations in combination with multiple chronic diseases when identifying patients for care models or care management programs.

Lisa is a turnaround expert who excels in navigating unsteady, complex, and ambiguous environments. She has provided C-suite education to over 10,000 organizations in the home care sector for decades. Lisa’s trusted voice in the industry has been recognized for her ability to manage disruption, identify new growth and revenue opportunities, and develop high-level engagement strategies between home care and referral partnerships. Her contributions are instrumental in advancing the future of home care.


