INTERACTIVE FEATURES: When viewing this article on an electronic device, note that web addresses are live links. Just click the link to visit that web page.
Click for instructions for moving the PDF into Kindle, Nook, Apple iBooks, and Apple Library.
How This Opens-up Growth Opportunities
Alex Azar, Secretary of Health and Human Services, says the government “cannot just tinker around the edges of a rural healthcare system that has struggled for too long.”
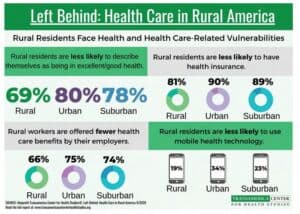
Rural areas are not only plagued by a shortage of providers, but lower incomes and higher incidents of chronic health conditions compared to urban areas. The 57 million rural residents are significantly more likely to die of heart disease, cancer or stroke compared to urban dwellers. Many rural facilities are closing and it’s harder to recruit physicians.
Last August, the Centers for Medicare & Medicaid Services Innovation Center (CMMI) announced its new Community Health Access and Rural Transformation (CHART) Model focused on improving financial sustainability, removing regulatory burdens, and enhancing access to care for rural residents.
The 84-page plan includes steps to expand the availability of telehealth services, to link residents to non-local healthcare providers. It directs the federal government to provide more than $8.7 million in grant funding for up to 29 providers to provide emergency care consults virtually to rural providers without specialists over the next four years.
The proposal would allow rural health clinics and federally qualified health centers to be allowed to furnish Medicare telehealth services and be reimbursed for virtual care at similar rates as comparable telehealth services under the Medicare Physician Fee Sched ule. CMS released the 2021 physician fee schedule in early August adding nine new permanent telehealth codes.
The new value-based payment model for rural healthcare providers ties payment to value, increases choice and lowers costs for patients, CMS said.
New Opportunities for Growth
 Providers interested in the CHART Model have two options for participation: the Community Transformation Track and the Accountable Care Organization (ACO) Transformation Track.
Providers interested in the CHART Model have two options for participation: the Community Transformation Track and the Accountable Care Organization (ACO) Transformation Track.
The Trump Administration is in vesting up to $75 million in seed money to allow up to 15 rural communities to participate in the Community Transformation Track. The investment allows for the implementation of care delivery reform, provides predictable capitated payments, and offers operational and regulatory flexibilities. The model starts in the summer of 2021.
Providers can pursue care transformation such as expanding telehealth to allow the beneficiary’s place of residence to be an originating site and waiving certain Medicare hospital conditions of participation to allow a rural outpatient department and emergency room to be paid as if they were classified as a hospital.
The model also allows participant hospitals to waive cost-sharing for certain Part B services and provide transportation support.
The Accountable Care Organization (ACO) Transformation Track offers an up-front investment. Providers participating in the ACO Transformation Track will enter into two-sided risk arrangements as part of the Medicare Shared Savings Program and may use all waivers that are available in the MSSP program.
CMS anticipates releasing a request for applications in the spring of 2021 and selecting up to 20 rural ACOs to participate in this track starting in January 2022.

Lisa is a turnaround expert who excels in navigating unsteady, complex, and ambiguous environments. She has provided C-suite education to over 10,000 organizations in the home care sector for decades. Lisa’s trusted voice in the industry has been recognized for her ability to manage disruption, identify new growth and revenue opportunities, and develop high-level engagement strategies between home care and referral partnerships. Her contributions are instrumental in advancing the future of home care.


