INTERACTIVE FEATURES: When viewing this article on an electronic device, note that web addresses are live links. Just click the link to visit that web page.
Click for instructions for moving the PDF into Kindle, Nook, Apple iBooks, and Apple Library.
Is Your Organization Ready to Take on Risk?
States are expanding value-based payments (VBP) in Medicaid and leveraging their Medicaid managed care programs to advance their payment reform goals.
According to Manatt Health, VBP policies vary across the country but the trends are clear:
- States are engaging their managed care contractors in VBP on multiple fronts.
- Increasingly mandating plan action on VBP and providing financial incentives.
- Imposing penalties tied to specific VBP goals.
A Manatt Health review of 39 states’ Medicaid managed care contracts and related sources found that 28 states require plans to engage in VBP with network providers; two other states explicitly encourage or otherwise incentivize plans to engage in VBP (See Figure 1).
How is Medicaid Managed Care Accelerating Value-Based Payments?
- Requiring managed care organizations (MCOs) to adopt a standardized value-based payment (VBP) model.
- Requiring MCOs to make a specific percentage of provider payments through approved VBP arrangements.
- Requiring the MCOs to move toward implementation of more sophisticated VBP approaches over the life of the contract.
- Requiring MCOs to actively participate in a multi-payer VBP alignment initiative.
Requiring MCOs to launch VBP pilot projects subject to state approval.
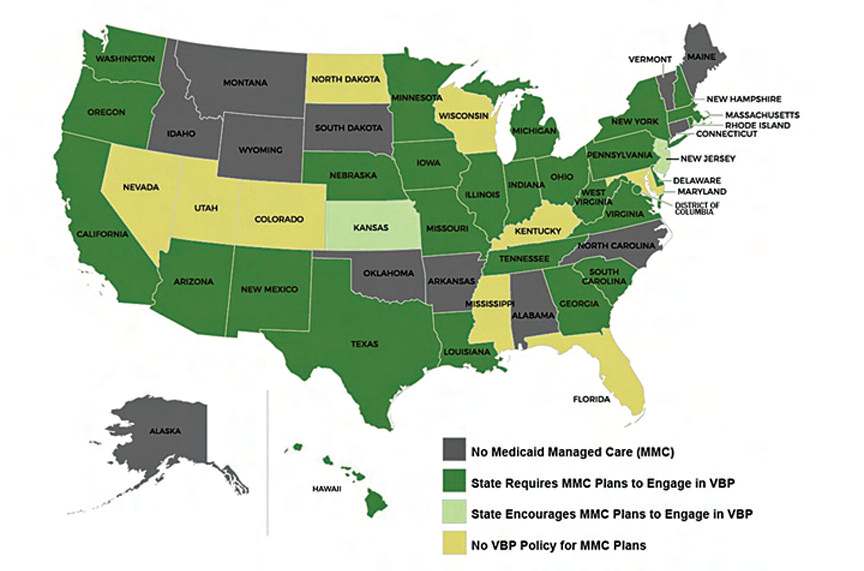
Figure 1. VBP Policies in State Medicaid Managed Care Programs

Lisa is a turnaround expert who excels in navigating unsteady, complex, and ambiguous environments. She has provided C-suite education to over 10,000 organizations in the home care sector for decades. Lisa’s trusted voice in the industry has been recognized for her ability to manage disruption, identify new growth and revenue opportunities, and develop high-level engagement strategies between home care and referral partnerships. Her contributions are instrumental in advancing the future of home care.


