Is 30 days the right interval for your organization to be measuring readmissions?
The Hospital Readmission Reduction Program aims to reduce excess readmissions among Medicare beneficiaries by applying financial penalties to hospitals with higher-than-expected 30-day all-cause readmission rates for acute myocardial infarction, chronic obstructive pulmonary disease, heart failure, and pneumonia. The two surgical procedures are coronary artery bypass and elective primary total hip and/or knee arthroplasty.
Key studies and data can help home-based care providers reduce readmissions, improve outcomes, and increase partnerships.
24.2% of Patients Discharged from a SNF to Home Were Readmitted to a Hospital Within 30 Days of a SNF Discharge
Readmission after a skilled-nursing facility (SNF) discharge following heart failure hospitalization is highest during the first two days home
Patients discharged with heart failure from a SNF to home face the highest risk of readmissions in the first two days after SNF discharge.
The study published in the Journal of the American Medical Directors Association reviewed Medicare claims data collected from more than 67,000 beneficiaries. A quarter of heart failure patients discharged from a hospital to a SNF then to home are readmitted to a hospital.
The research includes several key data points:
- 24.2% of patients discharged from a SNF to home were readmitted to a hospital within 30 days of a SNF discharge.
- The risk of readmission was highest in the first two days after a SNF discharge.
- Readmission risk declined with longer SNF length of stay.
Patients were followed for 30 days following a SNF discharge. The study categorized patients by SNF length of stay: 1-6 days, 7-13 days, and 14-30 days. For each group, the study modeled time to a composite outcome of unplanned readmission or death after a SNF discharge. The model examined 0-2 days and 3-30 days post- SNF discharge.
The Overall Conditions with the Most Frequent and Costly Readmissions
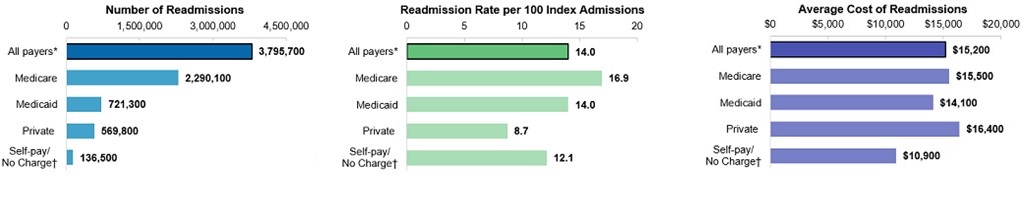
In 2018, there were 3.8 million 30-day all-cause adult hospital readmissions, with a 14% readmission rate and an average readmission cost of $15,200.
- Medicare accounted for 60.3% (2.3 million).
- Medicaid accounted for 19.0% (721,300).
In 2018, 20% of adult hospital readmissions were associated with four conditions at initial admission:
- Septicemia,
- Heart failure,
- Diabetes, and
- Chronic obstructive pulmonary disease.
Readmissions by Type of Payer, Cost, and Volume
Three sets of statistics, overall and by expected payer, on 30-day all-cause adult hospital readmissions: the number of readmissions, the readmission rate, and the average cost of readmissions.
Number, rate, and average cost of 30-day all-cause adult hospital readmissions, by expected payer, 2018
6 Key Findings About Readmissions
Is 30-days the right interval for your organization to be measuring readmissions? 30-day risk-standardized, all-cause, unplanned readmission rates are widely used to measure hospital penalties.
The optimal interval for capturing hospital-level variation in the risk of readmission appears to vary across conditions. For example, the acute myocardial infarction patients had the greatest increase in hospital-level variation after the tenth post-discharge day.
- Hospital-level readmissions were low at the 30-day cutoff.
- Readmissions were higher within the first several days after discharge, reaching the lowest point around seven days. This suggests that a five- to seven-day interval would better capture hospital-attributable readmissions, particularly when compared to intervals of 30, 60, or 90 days.
- The hospital quality signal is higher in the first five days after discharge than at longer time periods, such as 30 days. This suggests that hospitals’ practices with respect to care coordination and post-discharge follow-up could have the greatest impact within the first few days after discharge.
By Payer
- For both seven-day and 30-day readmissions, the rate of readmission was highest among patients with Medicare, followed by patients with Medicaid, no insurance, and private insurance.
- Among Medicaid patients who were discharged with congestive heart failure or schizophrenia at the index stay, nearly one in 10 stays resulted in readmission within 7 days.
- Among patients readmitted within 30 days of an index stay for septicemia or schizophrenia, uninsured patients were more likely than patients with insurance to return within seven days.
Another interesting point: Readmissions occurring after seven days appear to be more susceptible to geodemographic characteristics that reflect the inherent social and community-related factors in the patient’s environment after hospital discharge.

Lisa is a turnaround expert who excels in navigating unsteady, complex, and ambiguous environments. She has provided C-suite education to over 10,000 organizations in the home care sector for decades. Lisa’s trusted voice in the industry has been recognized for her ability to manage disruption, identify new growth and revenue opportunities, and develop high-level engagement strategies between home care and referral partnerships. Her contributions are instrumental in advancing the future of home care.
Other Articles You Might Enjoy
Improving Outcomes Between Home Care and Medicare Advantage Plans
Home care services have emerged as a critical strategy for improving health outcomes, reducing hospital readmissions, addressing both clinical and non-clinical needs, and improved patient satisfaction among Medicare Advantage beneficiaries.
Average 30-Day Readmission Rates by Medical Conditions
We provide critical readmission data about average readmission rates, condition-specific readmission rates, and hospitals with high and low readmission rates.
Hospital-at-Home Readmissions: Which Medical Conditions Created the Highest and Lowest Readmissions?
CMS’s report on the Acute Hospital Care at Home (AHCAH) initiative highlighted the highest and lowest readmission rates by medical conditions.