Clinical factors are responsible for just 20 percent of individuals’ health outcomes; the remainder can be attributed to health-related social needs (HRSNs).
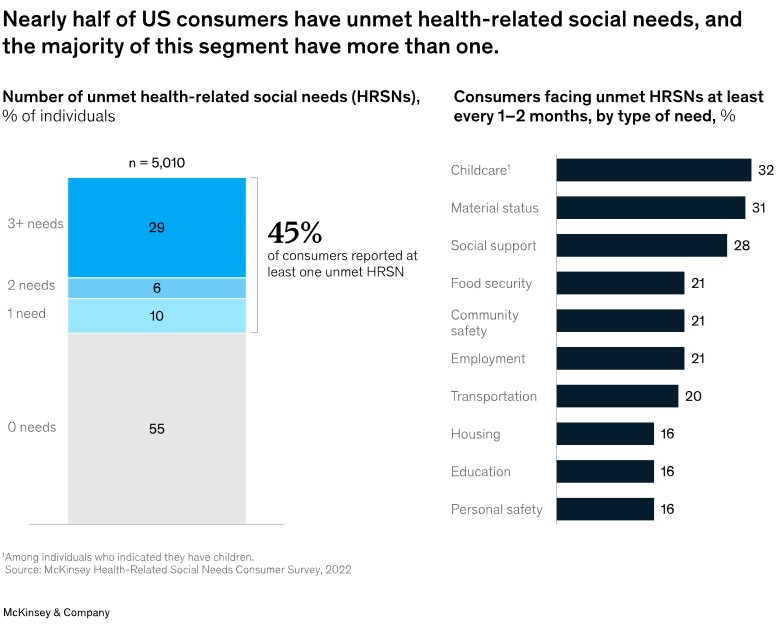
A survey of more than 5,000 US consumers highlights how HRSNs are evolving, their potential impact on healthcare use, preferences, and outcomes, and actions healthcare entities may consider to support consumers’ needs effectively.
Finding
- Consumers with HRSNs were more likely to report poor physical and mental health and barriers to accessing care.
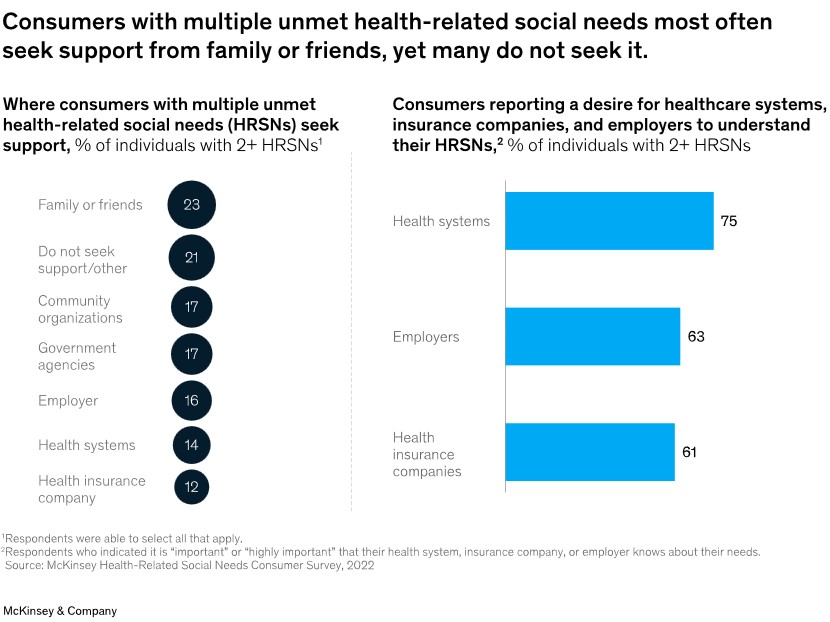
- Consumers with multiple HRSNs were more likely than other groups to report seeking support from family or friends, yet roughly 20 percent do not seek support.
- Consumers have expressed a strong desire for health systems, health insurance companies, and employers to gain a deeper understanding of their needs. This suggests that these entities have a significant role in meeting those needs and should consider stepping up their efforts.
Increasing recognition of the impact of these needs on consumers’ health and livelihoods is driving momentum across the healthcare ecosystem to integrate health and social care, creating opportunities for healthcare entities to design consumer-centric models of care tailored to individual needs and preferences.
Unmet HRSNs Create More Emergency Room Visits
Unmet HRSNs can lead to significant barriers to accessing necessary care. Shockingly, nearly 50 percent of consumers with multiple unmet HRSNs have reported not receiving all the care they need, compared to just 12 percent of those with none. This disparity is further underscored by the fact that consumers with two or more unmet HRSNs are three times more likely to visit the emergency room ‘frequently’ than those with none, a clear indication of the urgent need to address these issues.
Unmet HRSNs Affect All Payers
Unmet HRSNs cut across socioeconomic status. While consumers with lower incomes reported a greater prevalence of unmet HRSNs, nearly one-third of consumers with incomes of $100,000 to $149,999 also reported unmet HRSNs. Similarly, unmet HRSNs are prevalent across insurance types. While Medicaid, dual insurance, and uninsured individuals reported unmet HRSNs most heavily, two or more HRSNs affect nearly one-third of individuals reporting employer-sponsored insurance. This suggests screening for HRSNs should occur across patient segments, not just for Medicaid members.

Where are Consumers Going to Get Support?
When seeking HRSN-related support, consumers said they primarily go to family or friends (23 percent), followed by community organizations and government agencies (17 percent). Family, friends, and even community organizations may be a first resort, given the comfort, convenience, and speed of support. However, roughly 20 percent of consumers neither seek support nor look to alternative sources.
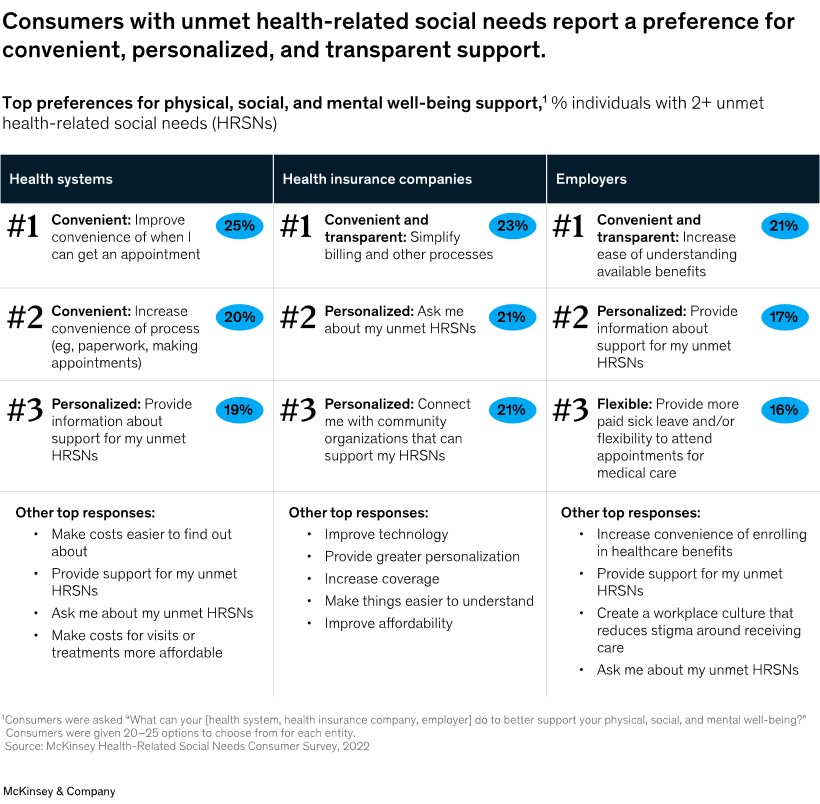
Top Consumer Preferences
Consumers identified convenience, personalization, and transparency when asked about their top preferences for support related to physical, social, and mental well-being. They highlighted a desire for better experiences in scheduling appointments, navigating billing and other processes, and understanding benefits offerings.
Consumer preferences, particularly in the context of health-related social needs (HRSNs), emerged as a significant theme. Consumers consistently expressed a desire for health systems, insurers, and employers to address their unmet HRSNs, indicating a clear opportunity for these entities to enhance their support offerings.
Beyond the top three preferences, other high-ranking preferences included flexibility, cost and affordability, and direct HRSN support (for example, medically tailored meals and other direct food provisions).
By aligning their strategies with consumer preferences, health insurance companies, health systems, employers, and others cannot only meet the needs of their consumers but also potentially improve health outcomes. This could involve designing consumer-centric solutions, fostering partnerships to address a wide range of needs, and tailoring support to caregivers and families.
Entities across the healthcare ecosystem can act to better meet consumers’ health-related social needs:
- Recognize that HRSNs affect consumers across socioeconomic levels and insurance types, and design programs to meet the needs of a variety of consumers.
- Design consumer-centric solutions (for example, with consumer input and involvement) to ensure they are tailored to be usable and effective (for example, matching personalized consumer preferences, ensuring transparency, prioritizing convenience, and reflecting cultural sensitivity).
- Explore a network of partnerships across the healthcare ecosystem to address a range of needs, given that consumers typically face multiple unmet needs.
- Consider the needs of caregivers and the family broadly – in addition to the individual – because roughly one-fourth of consumers reported seeking help from friends and family.
- Focus on improving convenience and personalization in HRSN programming, because this may significantly reduce hurdles to receiving care and other benefits.
The Remington Report team is a talented pool of researchers, analysts, and knowledge seekers providing excellence in home care content.




