In 2024, health and long-term care costs for people living with Alzheimer’s and other dementias are projected to reach $360 billion. Nearly 7 million American seniors are living with Alzheimer’s dementia, placing a huge strain on both personal caregivers and the U.S. health care system, according to a new Alzheimer’s Association report. Alzheimer’s disease was the fifth-leading cause of death among individuals aged 65 and older in 2021.
Thirty-six percent of individuals using home health services have Alzheimer’s or other dementias. Of Medicare beneficiaries aged 65 and older with Alzheimer’s or other dementias, 26% have at least one home health visit paid by Medicare during the year, compared with 8% of Medicare beneficiaries aged 65 and older without Alzheimer’s or other dementias and they use an average of 110 days of home care per year (including homemaker services and other services not covered by Medicare) compared with 64 days per year for individuals aged 65 and older without the disease. Receipt of home health services after hospital discharge has been shown to increase the likelihood of remaining in the community for at least 30 days after hospital discharge, with greater benefits from longer durations of home health care.
Readmission Rates
Among Medicare beneficiaries with Alzheimer’s or other dementias, 22% of hospital stays are followed by a readmission within 30 days. Although not directly comparable, one study of a random sample of Medicare beneficiaries from 50 U.S. hospital referral regions found an overall 30-day readmission rate of 18%. The proportion of hospital stays followed by a readmission within 30 days remained relatively constant between 2008 and 2018 for Medicare beneficiaries with Alzheimer’s and related dementias (23% in 2008 versus 22% in 2018.
Hospital Admissions
Dementia also made hospital admission more likely. Older adults with dementia were 1.34 times more likely to be admitted to the hospital after an ED visit than those without dementia, according to the study. In addition to having more hospital stays, older people with Alzheimer’s or other dementias have more skilled nursing facility stays per year than other older people.
In 2019, there were 518 hospital stays per 1,000 Medicare beneficiaries aged 65 and older with Alzheimer’s or other dementias compared with 234 hospital stays per 1,000 Medicare beneficiaries aged 65 and older without these conditions.
Overall, 32% of Medicare beneficiaries with Alzheimer’s or other dementias have at least one hospital discharge annually compared with 15% of beneficiaries without these conditions, with average hospital lengths of stay of 5.1 days versus 4.5 days, respectively. The most common reasons that people with Alzheimer’s dementia are hospitalized are not due to the disease itself, but for other reasons, including syncope (fainting), fall and trauma (26%), ischemic heart disease (17%), and gastrointestinal disease (9%). A study of inpatient hospitalizations of adults aged 60 and older found that those with Alzheimer’s dementia were at 7% greater risk of dying during the hospital stay and stayed nearly a day longer than individuals without Alzheimer’s dementia.
ED Visits
In a JAMA Neurology research letter, University of Michigan trialists reported that people with Alzheimer’s disease and related dementias (ARDS) make up approximately 7% of all emergency department (ED) visits from people 65 and older. Put another way, the study found that 25.3% of ED visits by older adults were made by individuals with dementia-related conditions, while only 15.5% of the population in this age group had dementia
One of the reasons emergency visits were so common in ARDS patients, the study found, is that they tend to have multiple chronic health conditions. Nearly three quarters of older dementia patients who made a trip to the ED had at least two additional documented medical issues. Only about 60% of older adults without dementia had other health complications that contributed to their emergency.
There were nearly 1.8 million emergency department visits for people with Alzheimer’s in 2021, representing 1.3% of all emergency department visits.878 There are 1,545 emergency department visits per 1,000 Medicare beneficiaries with Alzheimer’s or other dementias per year, including emergency department visits that result in a hospital admission.
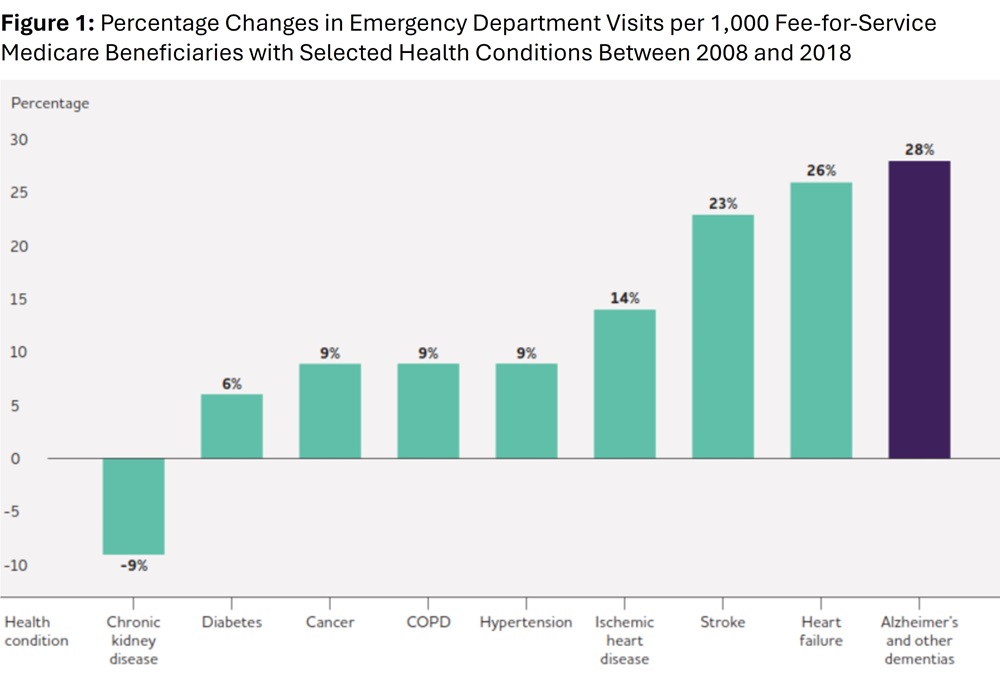
Although not directly comparable, there were 640 emergency department visits per 1,000 Medicare beneficiaries per year based on a review of utilization patterns of a subset of Medicare beneficiaries. Emergency department visits for people with Alzheimer’s or other dementias increased 22% between 2008 and 2018 (from 1,265 to 1,545 per 1,000 Medicare beneficiaries), exceeding the increases in emergency department visits for individuals with cancer, ischemic heart disease and heart failure, among others.
.
One group of researchers found that individuals with Alzheimer’s or another dementia seen in the emergency department are more likely to be admitted to the hospital or a nursing home from the emergency department than Medicare beneficiaries without Alzheimer’s or other dementias. Additionally, individuals with Alzheimer’s or other dementias are more likely to have at least one hospitalization, have at least one subsequent emergency department visit and be admitted to hospice in the 12 months following the initial emergency department visit.
Skilled Nursing Facilities
There are 188 skilled nursing facility stays covered by Medicare per 1,000 Medicare beneficiaries with Alzheimer’s or other dementias per year compared with 40 stays per 1,000 beneficiaries without these conditions – a rate nearly five times as high.413 Overall, 19% of Medicare beneficiaries with Alzheimer’s or other dementias have at least one skilled nursing facility stay annually compared with 4% of Medicare beneficiaries without these conditions.
The GUIDE Model
On July 31, 2023, the Centers for Medicare & Medicaid Services announced that beginning July 2024 it will support the Guiding an Improved Dementia Experience (GUIDE) Model until 2032.
The GUIDE Model features the provision of comprehensive dementia care coordination and management, caregiver education and support, and respite services. Individuals living with dementia and their caregivers will also have access to a 24/7 support line.
The GUIDE Model is unique in that it incentivizes providers to incorporate both the person with dementia and the caregiver (or caregivers) into the collaborative, multidisciplinary service approach. Critically, CMS will include policies to ensure that underserved communities have equal access to GUIDE Model services to address disparities in access to and quality of dementia care.
Through the GUIDE Model, participating organizations will offer dementia care programs that provide ongoing, longitudinal care and support for dually eligible Medicare and Medicaid people living with dementia and their caregivers, through an interdisciplinary team. Each team must include a knowledgeable and skilled care navigator to help people living with dementia and their caregivers access clinical and non-clinical services and supports, such as person-centered assessments and care plans, care coordination, caregiver training and education, meals, and transportation through community-based organizations, and 24/7 access to a support line.
CMS will evaluate an alternative payment for participating organizations, who must be Medicare Part B enrolled providers/suppliers and eligible to bill for Medicare Physician Fee Schedule services. To address racial health disparities and inequities in dementia care, CMS will actively seek out safety-net organizations that provide care to underserved communities to participate in the GUIDE Model and will provide financial and technical supports to ensure they can develop their infrastructure, improve their workforce and care delivery capabilities, and participate successfully.