Do You Know Which Principal Diagnosis has the Highest Rate of 30-Day Readmissions?
The federal government’s effort to penalize hospitals for excessive patient readmissions is ending its first decade with Medicare cutting payments to nearly half the nation’s hospitals.
In its 10th annual round of penalties, Medicare is reducing its payments to 2,499 hospitals, or 47% of all facilities. The average penalty is a 0.64% reduction in payment for each Medicare patient stay from October 2021 through September 2022.
The information provided in this article provides critical data to help manage readmissions.
In 2018, there were a total of 3.8 million adult hospital readmissions within 30 days, with an average readmission rate of 14 percent and an average readmission cost of $15,200.
“In its 10th annual round of penalties, Medicare is reducing its payments to 2,499 hospitals, or 47% of all facilities.”
Across all expected payers in 2018, there were 3.8 million readmissions.
- Medicare accounted for 60.3 percent (2.3 million)
- Medicaid accounted for 19.0 percent (721,300)
The overall readmission rate was 14.0 per 100 index admissions, with Medicare stays having the highest readmission rate (16.9 percent) and privately insured stays having the lowest readmission rate (8.7 percent). The average readmission cost was $15,200, ranging from $10,900 for self-pay/no charge stays to $16,400 for privately insured stays.
In 2018, 20 percent of adult hospital readmissions were associated with four conditions at index admission:
- Septicemia,
- Heart failure,
- Diabetes, and
- Chronic obstructive pulmonary disease (COPD)
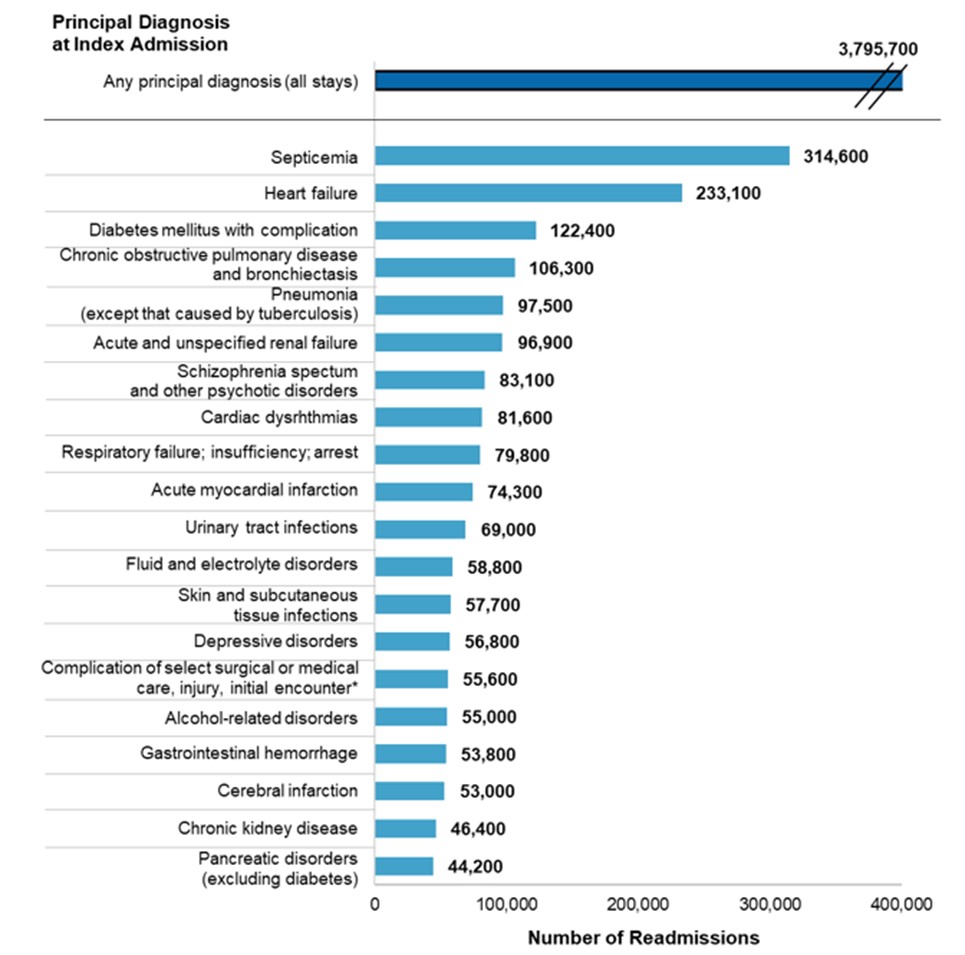
Hospital stays for septicemia at index admission had the highest number of 30-day all-cause readmissions in 2018 (314,600), accounting for 8.3 percent of all readmissions. The top four principal diagnoses at index admission—septicemia, heart failure, diabetes, and COPD—combined accounted for one in five readmissions.
Top 20 principal diagnoses with the highest number of 30-day all-cause adult hospital readmissions, 2018
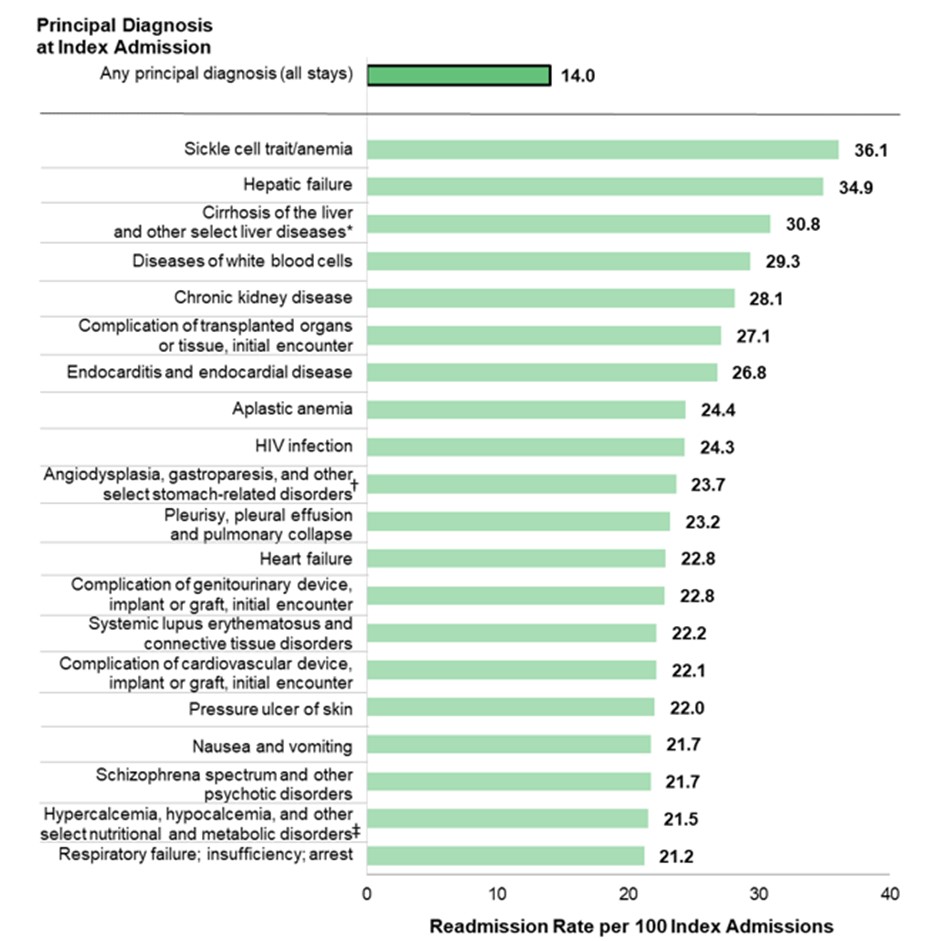
Which primary diagnosis had the highest rate of 30-day all-cause readmissions?
What Can Be Learned from This Data?
- Review your organization’s data based upon top clinical conditions to see if gaps or excessive readmissions.
- Evaluate technology best practices to front load conditions in need of 24/7 management.
- Review outcomes based upon clinical conditions.
- Evaluate readmissions by payer.
- Evaluate your organization’s clinical models for high-acuity patient oversight.
A must read to better understand 30-day vs. 7-day readmits
The Remington Report team is a talented pool of researchers, analysts, and knowledge seekers providing excellence in home care content.
Other Articles You Might Enjoy
Improving Outcomes Between Home Care and Medicare Advantage Plans
Home care services have emerged as a critical strategy for improving health outcomes, reducing hospital readmissions, addressing both clinical and non-clinical needs, and improved patient satisfaction among Medicare Advantage beneficiaries.
Average 30-Day Readmission Rates by Medical Conditions
We provide critical readmission data about average readmission rates, condition-specific readmission rates, and hospitals with high and low readmission rates.
Hospital-at-Home Readmissions: Which Medical Conditions Created the Highest and Lowest Readmissions?
CMS’s report on the Acute Hospital Care at Home (AHCAH) initiative highlighted the highest and lowest readmission rates by medical conditions.





