INTERACTIVE FEATURES: When viewing this article on an electronic device, note that web addresses are live links. Just click the link to visit that web page.
Click for instructions for moving the PDF into Kindle, Nook, Apple iBooks, and Apple Library.
How understanding the role of RTs can significantly impact chronic care management in the home
“In the acute care hospital, the RT is a well-respected team leader in respiratory care. Yet as soon as that patient is discharged, they suddenly lose that supportive RT expertise. RTs are underutilized in the post-acute setting because there currently is no payment mechanism to recognize essential RT services.”
“Until reimbursement reflects the strides that have been made in the technologies over the years, individuals with chronic respiratory disease that require home care stand to be at risk of not having access to much needed specialized care from respiratory therapists”, said Tom Kallstrom, Executive Director and Chief Executive Officer of the American Association for Respiratory Care (AARC). “This is especially prevalent now that Medicare has added noninvasive ventilators to competitive bidding,” he added.
According to Anne Marie Hummel, the Associate Executive Director of Advocacy and Government Affairs at the American Association for Respiratory Care (AARC), respiratory therapists are serving on the front line combating COVID-19 and saving lives on a daily basis. It is important now, more than ever, that Americans receive the care they require in their home without exposing themselves to the virus unnecessarily, and by ensuring hospital resources are reserved for those most in need. The AARC has engaged the Administration and Congress in lifting waivers that would allow respiratory therapists to be telehealth practitioners temporarily for the duration of the national public health emergency. Unfortunately, when the nation needs them most, respiratory therapists are not included among those professionals who can furnish telehealth services. By adding them to the roster of telehealth practitioners, respiratory therapists would be able to:
- Keep at-risk individuals out of hospitals by addressing the usual non-COVID-19 related respiratory conditions (e.g., flu, pulmonary infections, asthma attacks, COPD exacerbations, etc.).
- Expand their expertise and access, especially to individuals living in rural areas, by providing evaluation and assessment of the patient’s respiratory needs without face-to-face visits.
- Avoid the need to put high at-risk patients with underlying respiratory conditions in the emergency department or hospital by teaching self-management techniques to lessen their exposure to COVID-19 positive patients.
Change is Needed
With Chronic Obstructive Pulmonary Disease (COPD), the 4th leading cause of death and one of the costliest conditions relative to hospital readmissions, it is unconscionable that respiratory therapists — specialized health care professionals trained in cardiopulmonary care – are not paid directly for their clinical support in the home through the Durable Medical Equipment (DME) providers. This glaring oversight is due to Medicare’s interpretation that the DMEPOS benefit is about paying for the equipment only, not the clinical care that is essential for individuals to breathe and who require respiratory equipment to meet their daily needs.
- We contend that RT visits should have their own service reimbursement code and professional fee schedule, and not be considered a part of the indirect costs of the rental of a piece of equipment.
- RTs are skilled in providing training in respiratory care skills for ventilator patient to primary caregivers in the home, and LVNs or LPNs nursing staff in skilled nursing facilities or rehab centers. Skilled nursing facilities provide post-surgical recovery and rehabilitation in addition to long-term care. Caring for much higher acuity patient than ever before, RTs from the DME can do onsite assessments and respiratory case management tailored for each patient’s needs. The reimbursement for these services is usually borne by the facility itself.
“Unfortunately, decades ago, Medicare defined the scope of home health agencies to include only reimbursable disciplines: RN, OT, PT, ST, MSW, AND HHAs. Medicare did not recognize the expertise of RTs at that time. Fast forward to 2020, and the magnitude of COVID 19 patients, as well as the increased acuity of home patients should result in much better support for need RT skills.”
– Terry Racciato, RN PHN
In the acute care hospital, the RT is a well-respected team leader in respiratory care. Yet as soon as that patient is discharged, they suddenly lose that supportive RT expertise. RTs are underutilized in the post-acute setting because there currently is no payment mechanism to recognize essential RT services. The RTs expertise as part of the post-acute or home care case management team would allow other disciplines to securely practice at the top of their license, and contributing their own complementary expertise to the care team. The RTs have become the post-acute care or home care team respiratory case manager by default, especially when the home health agency has already discharged the home care patient. Over 80 % of all the DME home care patients are no longer being seen by a home health agency.
Unfortunately, decades ago, Medicare defined the scope of home health agencies to include only reimbursable disciplines: RN, OT, PT, ST, MSW, AND HHAs. Medicare did not recognize the expertise of RTs at that time. Fast forward to 2020, and the magnitude of COVID-19 patients, as well as the increased acuity of home patients should result in much better support for need RT skills.
For decades, respiratory therapists have made significant contributions to the well-being of those individuals who suffer from chronic respiratory disease while at the same time being faced with lack of acknowledgement through direct reimbursement for their services. These allied health professionals are specialists, educated and trained in all aspects of cardiopulmonary medicine. Their work in post-acute settings to evaluate, assess and monitor individuals on home mechanical ventilation (HMV), supplemental oxygen and positive airway pressure devices is invaluable.
Respiratory therapists are the essential health care providers employed in servicing patients on home mechanical ventilators (HMV). Ventilators require constant vigilance and adjustment as a patient’s needs change, as well as frequent maintenance. Invasive ventilators are among the most complex devices and require advanced knowledge and training to inform decision-making and to provide effective training for the caregiver and /or family members. Since a patient’s condition can deteriorate over time, it is imperative that the clinical expertise of a respiratory therapist make regular home visits, as well as being on call for emergencies at all times.
Patients who must use these ventilators are among the most medically fragile of the home care patient population. Ventilators are prescribed by the physician for patients suffering from specific and severe respiratory disorders. The ventilators initiate breaths, control intervals between breaths, inflate the patient’s lungs, and require frequent servicing, adjustments to the ventilator, and clinical assessment of the patient’s medical condition in order to assure: (1) that the patient’s safety and health are not being jeopardized, and (2) that the patient is maximizing the medical benefits of HMV.
The primary purposes of respiratory therapy patient visits are:
- To assess the patient’s physical condition and response to the treatment,
- To ensure the ventilator is set properly in response to the patient’s changing physical condition,
- To ensure the ventilator is operating properly in a home environment that supports the proper use of the ventilator itself, and
- To convey to the prescribing physician the patient’s clinical and overall response to the treatment.
In summary, we need Respiratory Therapists more than ever. At the same time, demand for caring for COVID-19 positive patients, DMEs have been decimated as an industry and forced to operate through increasingly-constrictive federal and state programs. Medicare’s competitive bid program compounded by the CURES Act[1] has resulted in 40 % of all of the DMEs in the U.S. closing, with more than 60% in California. The remaining DMEs have had to cut any and all overhead so that they can try and survive through this hostile reimbursement environment. RTs are considered an expensive luxury, rather than a necessity, for many DMEs who can no longer afford to provide the uncompensated overhead for the care service component with the draconian reimbursement cuts they have endured.
New York Governor Andrew Cuomo when referring to the health care shortage in the battle against COVID-19 stated on April 2, 2020, “You can’t expect that a health care system that was struggling before this added stress could possibly cover it. A fence is only as strong as its weakest link.”
We need to recognize that RTs have a tremendous role to play in the safety and care of our post-acute and home care patients. We also need to recognize the shortcomings of an archaic Medicare reimbursement system that hasn’t kept up with the technology and service settings to meet the needs of patients across the continuum.
In closing, we need a reimbursement code and fee schedule for the service component that a DME provides for its respiratory patients in order to assure that the RTs can provide the care and treatment within the scope of their unique specialty
States with the highest employment level in this occupation:
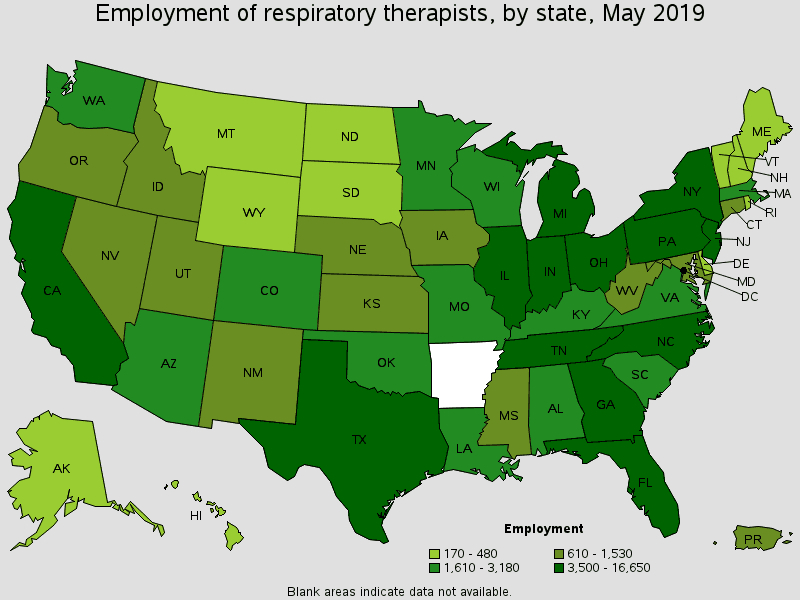
| State | Employment (1) | Employment per thousand jobs | Location quotient (9) | Hourly mean wage | Annual mean wage (2)the |
|---|---|---|---|---|---|
| California | 16,650 | 0.96 | 1.06 | $40.35 | $83,920 |
| Texas | 11,730 | 0.94 | 1.05 | $29.11 | $60,560 |
| Florida | 8,080 | 0.92 | 1.02 | $28.22 | $58,700 |
| Ohio | 6,190 | 1.14 | 1.26 | $27.93 | $58,090 |
| Pennsylvania | 5,930 | 1.00 | 1.12 | $27.69 | $57,600 |
Source: U.S. Bureau of Labor Statistics
Reference:
[1] States are required to pay less than the amount paid by Medicaid programs or face financial penalties from the federal government.

Terry Racciato, RN, PHN, is President, RAC & Associates, DBA SpecialCare, and President, CAMPS – The California Association of Medical Product Suppliers (CAMPS). CAMPS is a non-profit, statewide trade association representing the California HME industry.









