Healthcare is adopting integrated care approaches involving teams working across disciplines and sectors. We are seeing the transition to more team-based care because of the workforce shortage. For example, hospitals are reevaluating their nurse-to-patient ratios model. Instead of assigning one nurse to oversee a small group of patients, a team-based approach of several staff members who work at the top of their license care for a larger group of patients.
In care delivery models such as hospital-at-home, skilled-nursing facility at home, value-based care, managing social determinants of health, behavioral health, palliative care, and home-based primary care, the team-based approach is based upon:
Members come together as a whole to discuss their individual assessments and develop a joint service plan for the patient. Practitioners may blur some disciplinary boundaries but still maintain a discipline-specific base (for instance, aspects of functional assessments may be shared across disciplines). Teams integrate closer to complete a shared goal. (Ellis & Sevdalis, 2019).
2 Different Approaches to Team-Based Care
Though often used interchangeably, multidisciplinary and interdisciplinary care differ in their form and function.
Multidisciplinary Care Teams: A team composed of members from more than one discipline, offering patients a greater breadth of services. Team members work independently and in parallel, with each provider responsible for his or her own area. Communication between team members is formal, and team structure is often hierarchical with a designated leader overseeing the team.
Interdisciplinary Care Teams: A team of professionals from various disciplines participates in reaching a common goal, with each team member bringing his or her discipline’s expertise to the team. Team members work formally and informally, and information is shared in a systemic way among team members. An interdisciplinary team is collaborative and integrates each profession’s knowledge into the care plan.1
Each team member is encouraged to function to the fullest extent of their education, certification, and experience to reach optimal care outcomes.
How to Foster Effective Teams
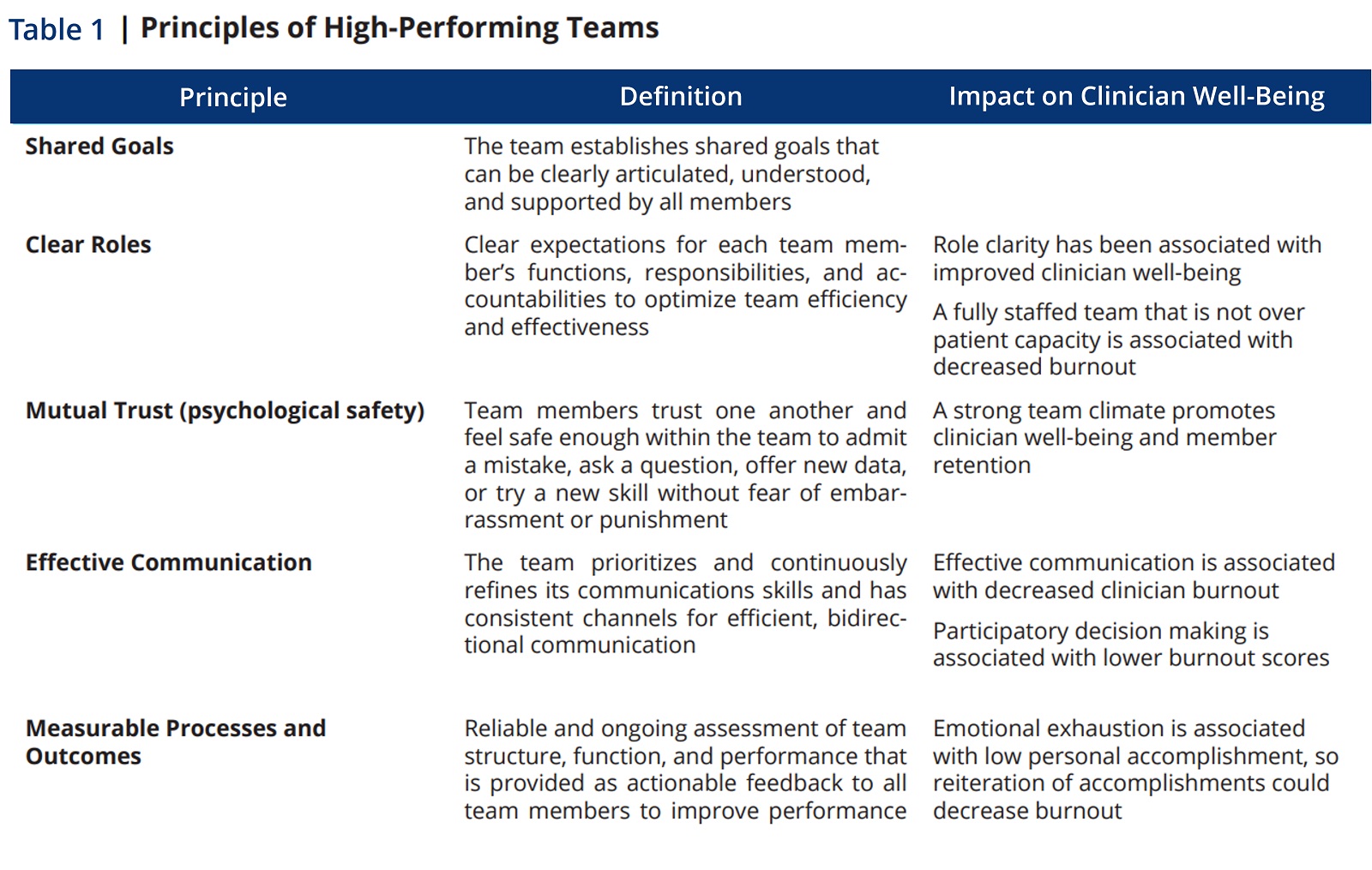
The National Academy of Medicine identified five core principles to enable care providers to foster effective care teams.
- Shared Goals. The team establishes shared goals that reflect the priorities of the patient and family. The goals are clearly articulated, understood, and supported by all team members.
- Clear Roles. There are clear expectations for each team member’s functions, responsibilities, and accountabilities.
- Mutual Trust. Team members trust one another and feel safe to admit a mistake, ask a question, offer new data, or try a new skill without fear of embarrassment or punishment.
- Effective Communication. The team prioritizes and continuously refines its communications skills and has consistent channels for efficient, bidirectional communication.
- Mutual Processes and Outcomes. A reliable and ongoing assessment of team structure, function, and performance is provided as actionable feedback to all team members to improve performance.
How Team-Based Care Reduces Clinician Burnout
As workforce issues continue to pose very real challenges, team-based care not only offers solutions to the workforce shortage, but also has the potential to enhance patient care in terms of quality and safety, expanded productivity, and improved job satisfaction by reducing workloads and preventing burnout.
High-functioning clinical teams are essential for the delivery of high-value healthcare and have been associated with:
- Decreased workloads
- Increased efficiency
- Improved quality of care
- Improved patient outcomes
- Decreased clinician burnout/turnover
In Table 1, we see the relationship between the principles of team-based care and the impact of improving clinician burnout.
The 4 Characteristics of Successful Teamwork
A team-based model of care strives to meet patient needs and preferences by actively engaging patients as full participants in their care while encouraging all healthcare professionals to function to the full extent of their education, certification, and experience.2
Successful Teamwork has 4 Key Characteristics
- A clear and compelling purpose or goal,
- An enabling social structure that facilitates teamwork,
- A supportive organizational context, and
- Expert teamwork coaching.3
Effective Teamwork Depends On:
- the team member’s psychological safety, defined as their ability to trust one another and feel safe enough within the team to admit a mistake, ask a question, offer new data, or try a new skill without fear of embarrassment or punishment, and
- allows team members to learn, teach, communicate, reason, think together, and achieve shared goals, irrespective of their individual positions or status outside the team4
Key Features of High-Functioning Healthcare Teams
- Shared team identity, value, and goals
- Leadership
- Defined and complimentary roles
- Continuity and regular meetings
- Adequate staffing
- Shared physical space
- Psychological safety
- Task sharing and shifting
- Effective help among team members
- Team coordination
- Open communication and mutual trust
- Constructive conflict resolution
- Observation and feedback
Team-based healthcare has been linked to improved patient outcomes and may also be a means to improve clinician well-being.5 The increasingly fragmented and complex healthcare landscape adds urgency to the need to foster effective team-based care to improve both the patient’s and team’s experience of care delivery.
Additional Insights to Combat Clinician Burnout
Footnotes
1ccnmtl.columbia.edu/projects/sl2/pdf/glossary.pdf.
2American College of Obstetricians and Gynecologists. 2016. Collaboration in practice: Implementing team-based care.
3Gordon, S., D. L. Feldman, and M. Leonard. 2014. Collaborative caring: Stories and reflections on teamwork in health care.
4Hackman, R. 2014. What makes for a great team? Washington, DC: American Psychological Association
5Welp, A., and T. Manser. 2016. Integrating teamwork, clinician occupational well-being, and patient safety—development of a conceptual framework based on a systematic review.
Other Articles You Might Enjoy
Best Practices for Effective Strategy Execution
Effective strategy execution is crucial for success, as even the most well-crafted strategies can fail if not properly implemented.
5 Reasons Why a 5-Year Strategic Plan May Pose Challenges
Five-year strategic plans in home care often encounter several challenges due to the dynamic nature of the industry.
Understanding Adaptive Leadership in Home Care’s Complex World
Adaptive leadership is not a fixed set of rules or practices; rather, it's a mindset and a skill set that empowers leaders to thrive in turbulent times.











