What Post-Acute Providers Need To Know
On July 29, 2019, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule that includes proposals to update payment policies, payment rates, and quality provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2020.
Background on the Physician Fee Schedule (PFS)
Payment is made under the PFS for services furnished by physicians and other practitioners in all sites of service. These services include, but are not limited to, visits, surgical procedures, diagnostic tests, therapy services, and specified preventive services.
In addition to physicians, payment is made under the PFS to a variety of practitioners and entities, including nurse practitioners, physician assistants, and physical therapists, as well as radiation therapy centers and independent diagnostic testing facilities.
Payments are based on the relative resources typically used to furnish the service. Relative Value Units (RVUs) are applied to each service for physician work, practice expense, and malpractice. These RVUs become payment rates through the application of a conversion factor. Payment rates are calculated to include an overall payment update specified by statute.
 Merit-based Incentive Payment System (MIPS), Moving To MIPS Value Pathways (MVPs)
Merit-based Incentive Payment System (MIPS), Moving To MIPS Value Pathways (MVPs)
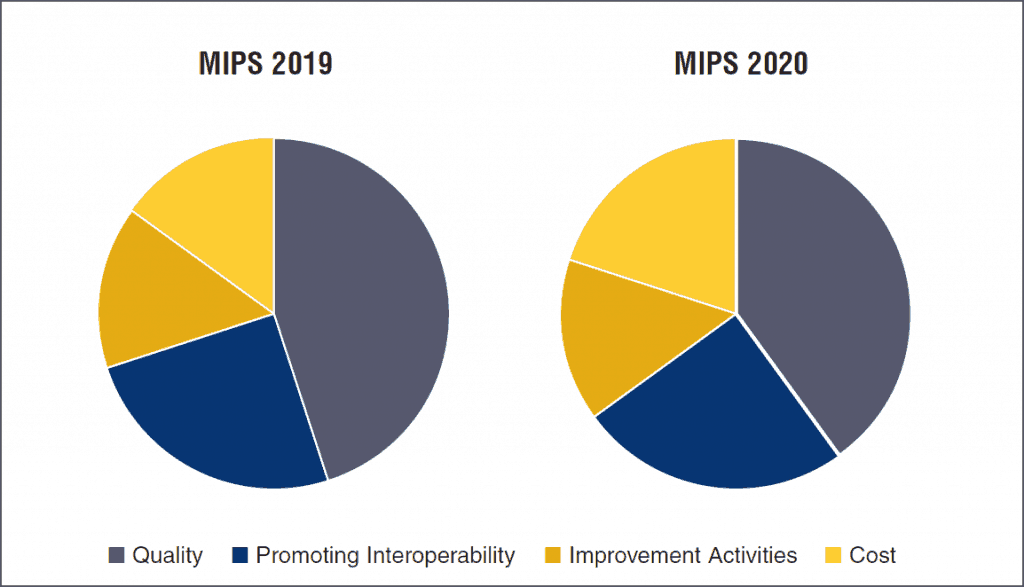
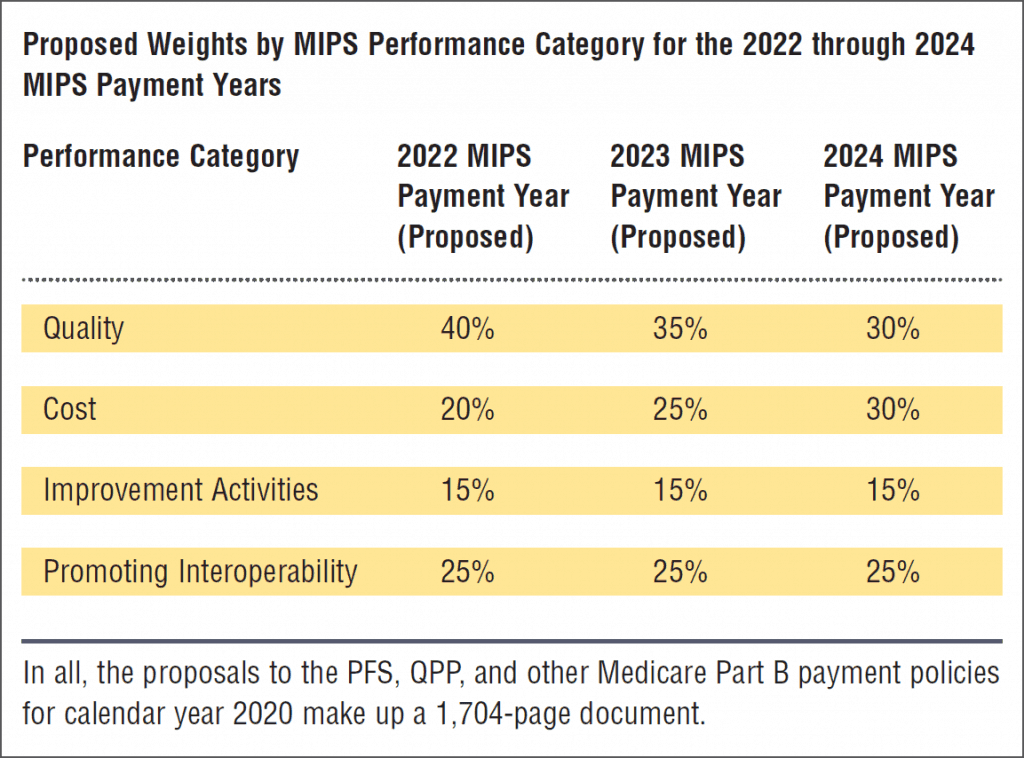
At the core of the proposed physician policy changes, CMS is seeking to improve the Quality Payment Program (QPP) under MACRA (the Medicare Access and CHIP Reauthorization Act of 2015) by streamlining the program’s requirements. The proposal calls for an easier way for clinicians to participate in CMS’ pay-for-performance program, the Merit-based Incentive Payment System (MIPS), which is one of two payment tracks within the QPP.
This new framework, called the MIPS Value Pathways (MVPs), beginning in the 2021 performance period, would move MIPS from its current state, which requires clinicians to report on many measures across the multiple performance categories, such as Quality, Cost, Promoting Interoperability and Improvement Activities, to a system in which clinicians will report much less.
Under MVPs, clinicians would report on a smaller set of measures that are specialty-specific, outcome-based, and more closely aligned to Alternative Payment Models (APMs). MVPs will connect activities and measures from the four existing MIPS performance categories that are relevant to the population they are caring for a specialty or medical condition, according to CMS.
Per the proposal, “MVPs would utilize sets of measures and activities that incorporate a foundation of promoting interoperability and administrative claims-based population health measures and layered with specialty/condition specific clinical quality measures to create both more uniformity and simplicity in measure reporting. The MVP framework will also connect quality, cost, and improvement activities performance categories to drive toward value; integrate the voice of patients; and reduce clinician barriers to movement into Advanced APMs.”
 2020 Billing and Coding Changes
2020 Billing and Coding Changes
Evaluation & Management Codes
For 2019, CMS finalized changes to simplify billing and coding requirements for certain office-based visits known as evaluation and management (E/M) services, respond to longstanding criticism that they were burdensome and overly complicated. Changes, the first to the E/M framework in more than 20 years, aim to give clinicians new flexibility to consider time with the patient or medical decision-making in how they code an E/M visit, so they could focus more closely on what is clinically relevant and medically necessary for the patient.
The proposed changes for 2020 would build on these policies by paying clinicians across all specialties for the time they spend treating the growing number of patients with greater needs and multiple medical conditions, through increasing the value of E/M codes for office/outpatient visits and providing enhanced payments for certain types of visits. “This is especially important to certain specialists that spend significant time managing patients with multiple co-morbidities, such as diabetes and heart disease,” the agency stated.
Chronic Care Management
CMS is proposing to take steps to help clinicians better manage chronically ill patients, particularly during their transition from hospital to home. The proposed rule would increase payments to practitioners for time spent on care management after a patient leaves the hospital ensuring proper follow-up and continuity of care for patients.
And, for the first time, CMS is proposing to pay for care management services for patients with a single, high-risk chronic condition such as diabetes or high blood pressure. CMS is also proposing to pay clinicians more for additional time spent on care management activities for patients suffering from multiple chronic conditions.
Opioid Treatment
The proposed rule also calls for expanded Medicare coverage to pay opioid treatment programs (OTPs) for delivering Medication-Assisted Treatment (MAT) to people with Medicare suffering from opioid use disorder (OUD). Opioid Treatment Programs (OTPs) are programs or providers that provide a range of services to people with opioid use disorder, including medication-assisted treatment and counseling. OTPs must be accredited by the Substance Abuse and Mental Health Services Administration (SAMHSA), and CMS is also proposing to make a new monthly bundled payment to practitioners for management and counseling involving MAT for patients with opioid use disorder.
2020 Proposed Payment Provisions: What Post-Acute Organizations Should Know
Medicare Telehealth Services
For CY 2020, the proposal adds the following codes to the list of telehealth services: HCPCS codes GYYY1, GYYY2, and GYYY3, which describe a bundled episode of care for treatment of opioid use disorders.
Chronic Care
CMS is proposing to consolidate the Medicare-specific add-on code for office/outpatient E/M visits for primary care and non-procedural specialty care finalized in the CY 2019 PFS final rule for implementation in CY 2021 into a single code describing the work associated with visits that are part of ongoing, comprehensive primary care and/or visits that are part of ongoing care related to a patient’s single, serious, or complex chronic condition.
Physician Supervision Requirements for Physician Assistants (PAs)
CMS is proposing to modify regulation on physician supervision of PAs to give PAs greater flexibility to practice more broadly in the current health care system in accordance with state law and state scope of practice. In the absence of State law governing physician supervision of PA services, the physician supervision required by Medicare for PA services would be evidenced by documentation in the medical record of the PA’s approach to working with physicians in furnishing their services.
Care Management Services
CMS is proposing to increase payment for Transitional Care Management (TCM), which is a care management service provided to beneficiaries after discharge from an inpatient stay or certain outpatient stays.
The proposal has a set of Medicare-developed HCPCS G codes for certain Chronic Care Management (CCM) services. CCM is a service for providing care coordination and management services to beneficiaries with multiple chronic conditions over a calendar month service period. The proposal replaces a number of the CCM codes with Medicare-specific codes to allow clinicians to bill incrementally to reflect additional time and resources required in certain cases and better distinguish complexity of illness as measured by time. The proposal also adjusts certain billing requirements and elements of the care planning services. These changes would also reduce burden associated with billing the complex CCM codes.
Recognizing that clinicians across all specialties manage the care of beneficiaries with chronic conditions, the proposal creates new coding for Principal Care Management (PCM) services, which would pay clinicians for providing care management for patients with a single serious and high risk condition.
Bundled Payment Concept Under the PFS
CMS is seeking comment on opportunities to expand the concept of bundling to improve payment for services under the PFS and more broadly align PFS payment with the broader CMS goal of improving accountability and increasing efficiency in paying for the health care of Medicare beneficiaries. CMS says that the statute, while requiring CMS to pay for services on the basis of the resources required to furnish the service, allows considerable flexibility for improving the efficiency of health service delivery within the PFS.
Bundled Payments under the PFS for Substance Use Disorders
In the CY 2019 PFS proposed rule, CMS sought comment on creating a bundled episode of care for management and counseling treatment for substance use disorders. In response to comments received, CMS is proposing to create new coding and payment for a bundled episode of care for management and counseling for Opioid Use Disorder (OUD).
The new proposed codes describe a monthly bundle of services for the treatment of OUD that includes overall management, care coordination, individual and group psychotherapy, and substance use counseling. One code describes the initial month of treatment, which would include administering assessments and developing a treatment plan; another code describes subsequent months of treatment; and an add-on code describes additional counseling.
CMS is proposing that the individual psychotherapy, group psychotherapy, and substance use counseling included in these codes could be furnished as Medicare telehealth services using communication technology as clinically appropriate. CMS is also seeking comment on bundles describing services for other Substance Use Disorders (SUDs) and on the use of Medication-Assisted Treatment (MAT) in the emergency department setting, including initiation of MAT and the potential for either referral or follow-up care, as well as the potential for administration of long-acting MAT agents in this setting, to help inform whether we should consider proposing to make separate payment for such services in future rulemaking.
Therapy Services
In the CY 2019 PFS final rule, in accordance with amendments to the Medicare law, modifiers were established to identify therapy services that are furnished in whole or in part by physical therapy (PT) and occupational therapy (OT) assistants. The proposal also established that the statutory reduced payment rate for therapy assistant services, effective beginning for services furnished in CY 2022, does not apply to services furnished by critical access hospitals because they are not paid for therapy services at PFS rates.
Medicare Shared Savings Program
CMS is soliciting comment on how to potentially align the Medicare Shared Savings Program quality performance scoring methodology more closely with the Merit-based Incentive Payment System (MIPS) quality performance scoring methodology. CMS recognizes that accountable care organizations (ACOs) and their participating providers and suppliers dedicate resources to performing well on quality metrics.
CMS believes that aligning quality metrics across programs will reduce burden and will allow ACOs to more effectively target their resources toward improving care.
Stark Advisory Opinion Process
CMS issues written advisory opinions on a case-by-case basis about whether a physician referral for certain health services is prohibited under Section 1877 of the Social Security Act (the “Stark Law”). Last year, CMS issued a Request for Information (RFI) to gather public input on how to address unnecessary burden created by the physician self-referral law, focusing in part on how it may impede care coordination, a key aspect of value-based healthcare.
In response to the RFI, many health systems and provider groups urged CMS to update the regulations governing its advisory opinion process on physician referrals to reduce provider burden and uncertainty around compliance with the Stark Law. For updates to Stark Reform Laws see: https://remingtonreport.com/intelligence-resources/futurefocus/.
Remington’s Takeaway
The Focus on Chronic Care Management Under MIPs
- Readmission Reduction: Hospital costs account for 1/3 of spending in U.S. healthcare. Two best practices have emerged to reduce unnecessary use of the hospital: chronic care management (CCM) and transitional care management (TCM).
- Chronic Care Management (CCM): Chronic care management (CCM) prevents hospital admissions. The purpose of CCM is to empower patients to better understand and better control their condition(s).
- Transitional Care Management (TCM): Transitional Care Management (TCM) prevents readmissions. The purpose of TCM is to prevent gaps in care as patients transition from the inpatient to the outpatient setting. Medicare’s TCM guidelines include: 1) interactive contact within 2 days of discharge, 2) a face-to-face visit within 7 or 14 days, and 3) other non-face-to-face services that you would expect. Two of six non-face-to-face services include:
- Obtaining and reviewing discharge information
- Identifying and following up on outstanding orders
- Preventing Unnecessary Use of the Emergency Department (ED): Approximately 30% of all ED visits in the U.S. are for non-emergent causes. Treatment from an ED costs 10x as much as similar care provided in less expensive setting.
- 24/7 Nurse Availability: Immediate access to a clinical team prevents patients from using unnecessary services or necessary services from unnecessary settings like an ED. Patients that can call a nurse line first can reduce ED visits when appropriate.

Lisa Remington is widely recognized as one of the foremost futurists in the home care industry, focusing on healthcare trends and disruptive innovation. She serves as the president and publisher of the Remington Report magazine and is also the President of Remington’s Think Tank Strategy Institute. Lisa provides strategic advice and education to over 10,000 organizations, assisting them in developing transformative strategies for growth and their future implications. She closely monitors complex trends and forces of change to develop effective strategic approaches.









