INTERACTIVE FEATURES: When viewing this article on an electronic device, note that web addresses are live links. Just click the link to visit that web page.
Click for instructions for moving the PDF into Kindle, Nook, Apple iBooks, and Apple Library.
Is Your Organization Ready to Take on Risk?
States are expanding value-based payments (VBP) in Medicaid and leveraging their Medicaid managed care programs to advance their payment reform goals.
According to Manatt Health, VBP policies vary across the country but the trends are clear:
- States are engaging their managed care contractors in VBP on multiple fronts.
- Increasingly mandating plan action on VBP and providing financial incentives.
- Imposing penalties tied to specific VBP goals.
A Manatt Health review of 39 states’ Medicaid managed care contracts and related sources found that 28 states require plans to engage in VBP with network providers; two other states explicitly encourage or otherwise incentivize plans to engage in VBP (See Figure 1).
How is Medicaid Managed Care Accelerating Value-Based Payments?
- Requiring managed care organizations (MCOs) to adopt a standardized value-based payment (VBP) model.
- Requiring MCOs to make a specific percentage of provider payments through approved VBP arrangements.
- Requiring the MCOs to move toward implementation of more sophisticated VBP approaches over the life of the contract.
- Requiring MCOs to actively participate in a multi-payer VBP alignment initiative.
Requiring MCOs to launch VBP pilot projects subject to state approval.
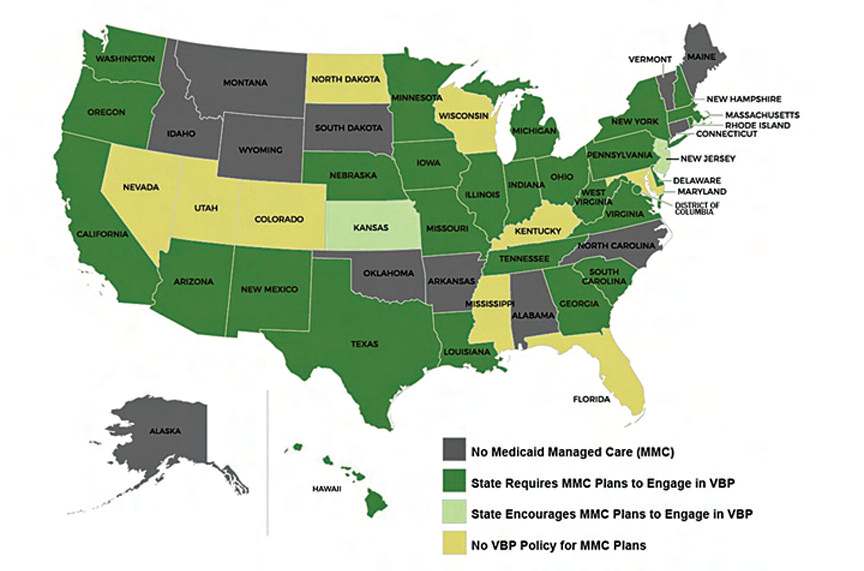
Figure 1. VBP Policies in State Medicaid Managed Care Programs

Lisa Remington is widely recognized as one of the foremost futurists in the home care industry, focusing on healthcare trends and disruptive innovation. She serves as the president and publisher of the Remington Report magazine and is also the President of Remington’s Think Tank Strategy Institute. Lisa provides strategic advice and education to over 10,000 organizations, assisting them in developing transformative strategies for growth and their future implications. She closely monitors complex trends and forces of change to develop effective strategic approaches.









