Why Do ACOs Limit Home-Based Care?
A recent study in the Journal of Managed Care was an eye-opener when it comes to better understanding home-based care from an ACO perspective.
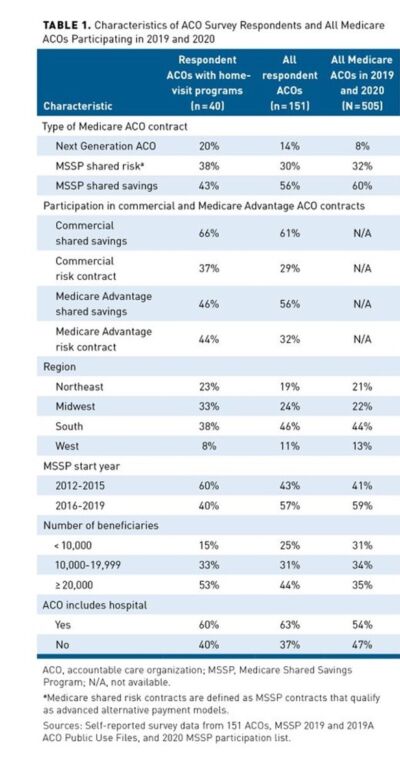
The study surveyed 151 participating in the Medicare Shared Savings Program (MSSP) or Next Generation ACO (NGACO) model as of July 1, 2019. Forty-four percent of respondents were enrolled in a Medicare ACO track with downside risk compared with 40% of all Medicare ACOs. Table 1. Twenty-five percent of ACOs had formal home-based programs, 25% offered occasional home visits, and 17% were actively developing new programs. The most common program was home-based primary care. Two-thirds has fewer than 500 visits.
Areas of Concern for ACOs
The concerns of many ACOs were focused on reimbursement. While ACOs deliver a diverse array of home-visit services including primary care, acute medical care, palliative care, care transitions, and interventions to address social determinants of health, many services provided are not billable, and therefore ACO leaders are hesitant to fund expansions without convincing evidence of ROI.
Funding sources included direct billing for services, health system subsidies, and ACO shared savings. “A majority of respondents expressed interest in expanding services but were concerned about their ability to demonstrate a return on investment (ROI), which was reported as a major or moderate challenge by three-quarters of respondents,” the study said.
Three key points were made in the study.
- With Medicare’s expansion of mandatory downside risk, more ACOs are considering home-based programs.
- ACO managers are hesitant to expand these programs unless they can demonstrate a return on investment.
- Expanding home-visit waivers to all risk-bearing Medicare ACOs and covering telehealth for patients receiving home-based primary care would improve these programs’ financial viability.
Looking Forward: Questions for Organizations
CMS’s commitment to value-based care has never been stronger. It announced a goal last year to move all Medicare beneficiaries into shared savings programs. Today, nearly one in five Medicare enrollees will be treated by ACOs Shared Savings programs.
More ACOs are also taking on risk this year, with 59% in two-sided risk tracks compared to 41% in 2021. An ACO agrees to meet certain spending and quality targets. The ACO gets a share of any savings it produces for meeting the targets but must repay Medicare for falling short.
This is an important time for your organization to prepare to partner based on risk. Questions to discuss.
- Does your organization understand the infrastructure of different types of ACOs? For example, in a Next Generation ACO quality of care is measured on 23 measures in four key domains, including patient/caregiver experience, care coordination/patient safety, preventive health and at-risk populations.
- How is/can your organization be partnering on ROI?
- What is your readiness for risk?

Lisa Remington is president and publisher of the Remington Report magazine and President of Remington’s Home Care Leadership Think Tank. She has worked with more than 10,000 organizations in both a consultancy role and an educator. Lisa monitors the complex key trends and forces of change to develop a correct strategic approach to de-risk decision-making and create sustainable futures across the healthcare continuum.
Other Articles You Might Enjoy
Message From Lisa Remington
May/June 2024 Issue
FREE CONTENT The home care industry lies at the center of chronic care management. It holds the key to reducing the overall cost of care, minimizing readmissions, emergency department visits, and offering value propositions that align with partnerships involving hospitals, health systems, ACOs, payers, and Medicare Advantage Plans.
Assessing the Effectiveness of Chronic Care Management Services
May/June 2024 Issue
SUBSCRIBER CONTENT Are you aware that both Medicare and Medicare Advantage beneficiaries are eligible for the Chronic Care Management program? It presents a remarkable opportunity to offer comprehensive care to those grappling with multiple chronic conditions. However, despite the widespread prevalence of chronic illnesses among Medicare beneficiaries, only a fraction is using the program. Which physicians are leveraging the program most frequently? What are the challenges?
Surprising Medical Conditions Dominating Home Healthcare Expenditure
May/June 2024 Issue
SUBSCRIBER CONTENT It's often assumed that heart disease ranks highest for medical condition expenditure in home healthcare. Get ready to be surprised by the real leader in medical expenditure.













