INTERACTIVE FEATURES: When viewing this article on an electronic device, note that web addresses are live links. Just click the link to visit that web page.
Click for instructions for moving the PDF into Kindle, Nook, Apple iBooks, and Apple Library.
Amid COVID-19 pandemic, 91% of Medicare Advantage beneficiaries using telehealth report favorable experiences while a record-setting 99% express satisfaction with their MA plan
With all the new conversations about technology, it will not surprise most home care providers that a new poll indicated high satisfaction from seniors using telehealth. Patient satisfaction surveys in home care have reflected that same result for the last decade!
Better Medicare Alliance (BMA), a research and advocacy organization supporting Medicare Advantage, released the results of their survey of more than 1,000 seniors on Medicare Advantage.
The survey, conducted between May 16-18, found near-unanimous satisfaction with Medicare Advantage (99%) while also reporting high favorability for telehealth (91%), strong trust in information provided by Medicare Advantage plans (84%), and few interruptions to health care services during the COVID-19 pandemic (73% saw no interruptions).
“We have heard a lot of conversation about telehealth in Beltway circles and these new findings offer evidence from seniors across the country that they, too, are learning to use these services. Our survey found that Medicare Advantage beneficiaries who try telehealth are overwhelmingly satisfied and 78 percent are willing to use it again,” said Allyson Y. Schwartz, President and CEO of the Better Medicare Alliance.
“At the same time, seniors’ satisfaction with Medicare Advantage has reached an all-time high of 99 percent – topping the previous record of 94 percent. Survey data shows that beneficiaries trust information provided from their doctors and health plan about the COVID-19 pandemic more than the news media or even family and friends. Beneficiaries are also highly confident in their ability to obtain a coronavirus test if needed – a finding we attribute to Medicare Advantage’s strong emphasis on coordinated and primary care.”
Schwartz concluded, “Together, these findings offer a comprehensive picture of the significant value that Medicare Advantage delivers to seniors in these difficult times, and of beneficiaries’ willingness to receive health care in new ways. We hope policymakers will take these findings to heart as they consider actions needed to provide security and stability for Medicare Advantage that 24.4 million Americans rely on today.”
Telehealth Key Findings
- 99% of respondents say they are satisfied with their Medicare Advantage coverage, including 64% who are very satisfied.
- Additionally, 94% are satisfied with their Medicare Advantage plan’s overall handling of the coronavirus, and 89% are satisfied with how their Medicare Advantage plan has kept them informed about their response to the coronavirus.
- A majority of seniors on Medicare Advantage (73%) have continued to receive care for their health care needs either in person or by telehealth, while 27% have experienced interruptions in health care during coronavirus.
- 68% of Medicare Advantage beneficiaries are confident that they would have access to a coronavirus test if needed.
- A majority of seniors on Medicare Advantage (79%) say they have received enough information about receiving health care during coronavirus, while 21% wish they received more information about receiving health care during COVID-19.
- Overall, half of seniors on Medicare Advantage (52%) are comfortable using telehealth services to receive health care, while 30% are uncomfortable, and 18% are unsure. A quarter (24%) have used telehealth services during the coronavirus to receive health care.
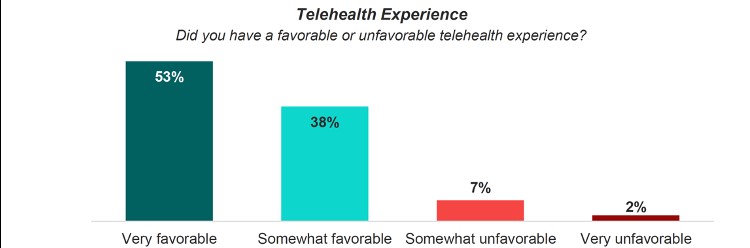
- Among those who have used telehealth services during the coronavirus pandemic, a strong majority (91%) had a favorable telehealth experience and 78% are likely to complete a medical appointment via telehealth again in the future.
Medicare Advantage Plans Expanding Telehealth
In May, the Centers for Medicare & Medicaid Services (CMS) finalized requirements that will increase access to telehealth for seniors in Medicare Advantage (MA) plans, expand the types of supplemental benefits available for beneficiaries with an MA plan who have chronic diseases, provide support for more MA options for beneficiaries in rural communities, and expand access to MA for patients with End Stage Renal Disease (ESRD). Together, the changes advance President Trump’s Executive Orders on Protecting and Improving Medicare for Our Nation’s Seniors and Advancing American Kidney Health as well as several of the CMS strategic initiatives.
“Among those who have used telehealth services during the coronavirus pandemic, a strong majority (91%) had a favorable telehealth experience and 78% are likely to complete a medical appointment via telehealth again in the future.”
Due to the June 1, 2020, MA and Part D bid deadlines for the 2021 plan year, CMS is finalizing a subset of the proposed policies before the MA and Part D plans’ bids are due. CMS plans to address the remaining proposals for plans later in 2020 for the 2022 plan year. CMS understands that the entire healthcare sector is focused on caring for patients and providing coverage related to coronavirus disease 2019 (COVID-19), and believe this approach provides plans with adequate time and information to design the best coverage for Medicare beneficiaries.
“CMS’s rapid changes to telehealth are a godsend to patients and providers and allows people to be treated in the safety of their home,” said CMS Administrator Seema Verma. “The changes we are making will help make telehealth more widely available in Medicare Advantage and are part of larger efforts to advance telehealth.”
Building on actions that the Trump Administration has taken to expand access to telehealth so beneficiaries can get care at home instead of traveling to a healthcare facility, the rule encourages MA plans to increase their telehealth benefits and increase plan options for beneficiaries living in rural areas. CMS is giving MA plans more flexibility to count telehealth providers in certain specialty areas (such as Dermatology, Psychiatry, Cardiology, Ophthalmology, Nephrology, Primary Care, Gynecology, Endocrinology, and Infectious Diseases) towards meeting CMS network adequacy standards. This flexibility will encourage plans to enhance their benefits to give beneficiaries access to the latest telehealth technologies and increase plan choices for beneficiaries residing in rural areas.
The rule gives beneficiaries with ESRD more coverage choices in the Medicare program. Previously, beneficiaries with ESRD were only allowed to enroll in MA plans in limited circumstances. The rule implements the changes made by the 21st Century Cures Act to give all beneficiaries with ESRD the option to enroll in an MA plan starting in 2021. This will give beneficiaries with ESRD access to more affordable Medicare coverage options that may include extra benefits such as health and wellness programs, transportation, or home-delivered meals that are not available in Medicare Fee-For-Service.
Hopefully, the support of CMS in advancing the use of telehealth for those covered by MA plans will also signal wider expansion and adoption of telehealth solutions for those covered by commercial health insurance plans as the value of telehealth has been battle-tested by the pandemic.