- In 2020, there were 5,058 hospices.
- Medicare hospice expenditures totaled $22.4 billion.
- In 2020, more than 1.7 million Medicare beneficiaries (including almost half of decedents) received hospice services.
- In 2020, the number of hospice providers increased by 4.5 percent, due to growth in the number of for-profit hospices, continuing a more than decade-long trend of substantial market entry by for-profit providers.
- Between 2019 and 2020, average lifetime length of stay among decedents grew from 92.5 days to 97.0 days, and the median length of stay was stable at 18 days.
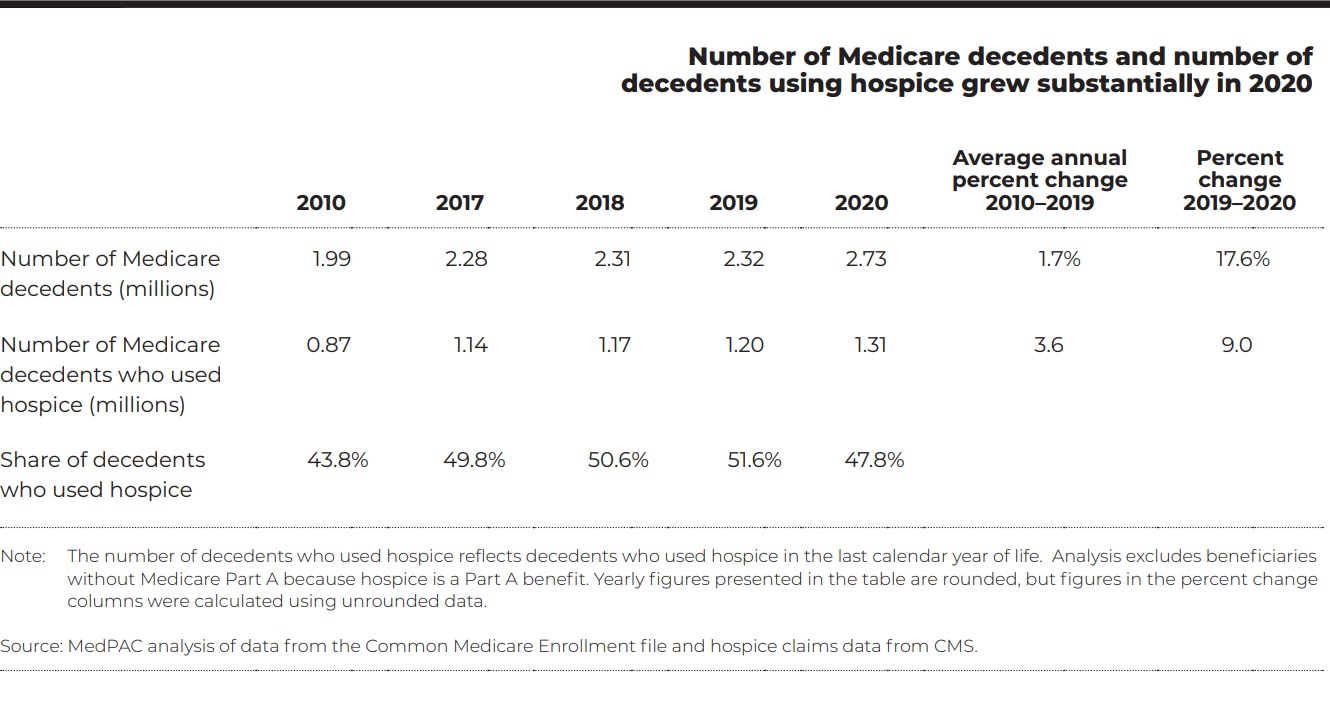
- Volume of services: In 2020, the number of beneficiaries using hospice services at the end of life continued to grow. However, the share of Medicare decedents using hospice declined between 2019 and 2020, from 51.6 percent to 47.8 percent, as deaths increased more rapidly than hospice enrollments.
Number of Medicare decedents and number of decedents using hospice grew substantially in 2020
- Cost growth: Between 2018 and 2020, hospice cost growth was generally modest. Average cost per day for routine home care, the level of care that accounts for more than 98 percent of hospice days, increased 0.5 percent between 2018 and 2019 and 1.2 percent between 2019 and 2020. In contrast, average cost per day for general inpatient care, inpatient respite care, and continuous home care, which are provided relatively infrequently, rose substantially in 2020.
- Aggregate Cap: The cap limits the total payments a hospice provider can receive in a year in aggregate. The aggregate cap functions as a mechanism that reduces payments to hospices with long stays and high margins. In 2019, about 19 percent of hospices exceeded the cap; their Medicare aggregate margin was about 22 percent before and 10 percent after application of the cap.

Other Articles You Might Enjoy
Message From Lisa Remington
March/April 2024 Issue
FREE CONTENT The surge in collaborations between home care providers and referral sources is creating fresh avenues for growth and fostering opportunities for deeper relationship-building. Fostering relationships involves cultivating meaningful connections and collaboration. The increase in referral partnerships between home care and referral partners can be attributed to seven key factors.
ACO MarketScan: Payments Shifting Care at Home Volume
March/April 2024 Issue
SUBSCRIBER CONTENT ACO MarketScan: What makes it crucial for home care providers to establish connections with ACOs? With more than half of Medicare beneficiaries enrolled in accountable care organizations, aiming for 100%, home care providers must craft compelling value propositions and engagement strategies to foster partnerships.
Hospital MarketScan: Hospital Outcome and Quality Measures
March/April 2024 Issue
SUBSCRIBER CONTENT Hospital MarketScan: A thorough grasp of hospital quality and outcomes proves highly advantageous for home care providers. Establishing and fortifying referral partnerships with hospitals and health systems necessitates a more comprehensive understanding of hospital outcomes and quality measures to enhance relationship building efforts.