-
 New choices to receive care at home centers on patients receiving acute level care in the home. Non-traditional care at home models is expanding into a new era. The twist to non-traditional programs is to keep care at home leadership?s eyes wide open about the impact to their organizations. Waivers are changing rules, policies have changed, and the role of who can care for patients in the home is transforming models. This article is free to 1-Year Classic and 2-Year Premium subscribers.
New choices to receive care at home centers on patients receiving acute level care in the home. Non-traditional care at home models is expanding into a new era. The twist to non-traditional programs is to keep care at home leadership?s eyes wide open about the impact to their organizations. Waivers are changing rules, policies have changed, and the role of who can care for patients in the home is transforming models. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 The invisible technology boundaries expand the rules of who can offer care in the home, how they will be paid, and it creates a less restrictive policy environment to deliver care at home. The opportunity to reshape care delivery and create a more efficient and cost-effective healthcare system is achievable because of the acceleration and adoption of technology. This article is free to 1-Year Classic and 2-Year Premium subscribers.
The invisible technology boundaries expand the rules of who can offer care in the home, how they will be paid, and it creates a less restrictive policy environment to deliver care at home. The opportunity to reshape care delivery and create a more efficient and cost-effective healthcare system is achievable because of the acceleration and adoption of technology. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 The question for leadership is how do you want to position your organization? As an integrator? Or as an aggregator? For care at home providers, the goal is to create a post-acute continuum model as patients transition from one care setting to another whether that be in-home personal care services, skilled home health, palliative care, or hospice. This article is free to 1-Year Classic and 2-Year Premium subscribers.
The question for leadership is how do you want to position your organization? As an integrator? Or as an aggregator? For care at home providers, the goal is to create a post-acute continuum model as patients transition from one care setting to another whether that be in-home personal care services, skilled home health, palliative care, or hospice. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Geographic direct-contracting model (GEO) is the latest CMS Center for Medicare and Medicaid Innovation (CMMI) model which allows Direct Contracting Entities to accept full financial risk for all traditional Medicare enrollees in their region. Three options enhance Medicare benefits and provide waivers for care in the home. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Geographic direct-contracting model (GEO) is the latest CMS Center for Medicare and Medicaid Innovation (CMMI) model which allows Direct Contracting Entities to accept full financial risk for all traditional Medicare enrollees in their region. Three options enhance Medicare benefits and provide waivers for care in the home. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
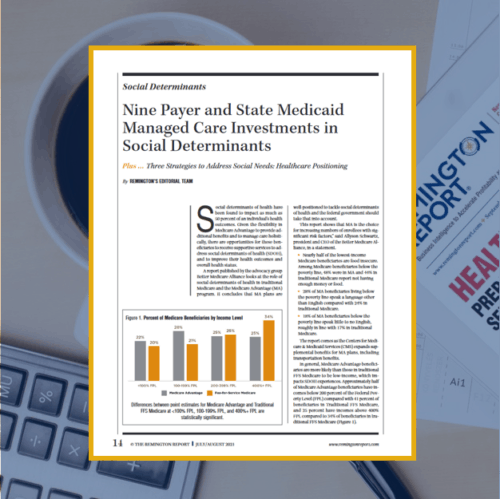
 A growing number of initiatives are expanding to address social determinants of health. Payers, health systems, community-based organizations, and government entities are partnering together to create statewide efforts to improve community health and social care. This article is free to 1-Year Classic and 2-Year Premium subscribers.
A growing number of initiatives are expanding to address social determinants of health. Payers, health systems, community-based organizations, and government entities are partnering together to create statewide efforts to improve community health and social care. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Expanding continuum of care services is an important strategy for future market positioning. We explore how providers, payers, and physicians are broadening services to expand partnership referrals, create innovation, and ensure sustainability. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Expanding continuum of care services is an important strategy for future market positioning. We explore how providers, payers, and physicians are broadening services to expand partnership referrals, create innovation, and ensure sustainability. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
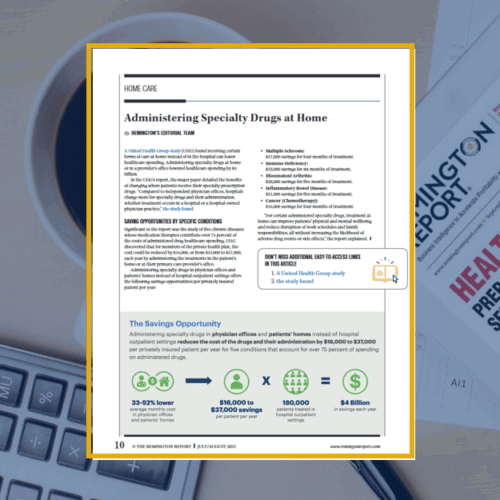
 New information will help your organization better align clinical services to reduce the cost of the highest medical conditions and their expenditures. The data can be used in conversations with various payer sources to align your organization’s services to reduce the cost of care and readmissions. This article is free to 1-Year Classic and 2-Year Premium subscribers.
New information will help your organization better align clinical services to reduce the cost of the highest medical conditions and their expenditures. The data can be used in conversations with various payer sources to align your organization’s services to reduce the cost of care and readmissions. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Payers, health systems, Private Equity firms, and SPAC’S acquisition of care at home companies are quickly changing market dynamics, and signaling change is ahead. This is a must-read to understand trends and insights reshaping the future. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Payers, health systems, Private Equity firms, and SPAC’S acquisition of care at home companies are quickly changing market dynamics, and signaling change is ahead. This is a must-read to understand trends and insights reshaping the future. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 The National Institute of Health advance care planning studies are focusing on the effectiveness of telehealth for patients receiving home-based palliative care and leveraging in home support services to engage patients in advance care planning. Learn more about the pilot studies supporting this research. This article is free to 1-Year Classic and 2-Year Premium subscribers.
The National Institute of Health advance care planning studies are focusing on the effectiveness of telehealth for patients receiving home-based palliative care and leveraging in home support services to engage patients in advance care planning. Learn more about the pilot studies supporting this research. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 The right of patients to choose providers has generated considerable conflict within the provider community. In this article, learn the four key legal sources supporting patient choice and actions your organizations and patients can take to have them enforced. This article is free to 1-Year Classic and 2-Year Premium subscribers.
The right of patients to choose providers has generated considerable conflict within the provider community. In this article, learn the four key legal sources supporting patient choice and actions your organizations and patients can take to have them enforced. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 A review of payment models under CMS’ Center for Medicare and Medicaid Innovation (CMMI) is quietly under review to decide if they will be implemented. Many of these models were popular with care at home providers. We provide insight into each of these payment models. This article is free to 1-Year Classic and 2-Year Premium subscribers.
A review of payment models under CMS’ Center for Medicare and Medicaid Innovation (CMMI) is quietly under review to decide if they will be implemented. Many of these models were popular with care at home providers. We provide insight into each of these payment models. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Your referral sources are the lifeblood of your organization. Ultimately, they will look for relationships with organizations that are easy to work with and that can deliver proven quality care. A new research report reveals the four frustrations felt by your referral sources. A roundtable of your peers’ weigh-in with solutions. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Your referral sources are the lifeblood of your organization. Ultimately, they will look for relationships with organizations that are easy to work with and that can deliver proven quality care. A new research report reveals the four frustrations felt by your referral sources. A roundtable of your peers’ weigh-in with solutions. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Payers are targeting their member populations that will benefit the most from at-home care. The center of their home health offerings is focused on high-cost patients, palliative care, diabetes, home care visits, telehealth, and at-home testing. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Payers are targeting their member populations that will benefit the most from at-home care. The center of their home health offerings is focused on high-cost patients, palliative care, diabetes, home care visits, telehealth, and at-home testing. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Strategies and actions to improve clinician experiences. Work/life balance is something nurses are constantly trying to achieve, and many nurses are falling short of that goal. What solutions are your peers using to combat burnout, achieve better nurse work/life balance, and improve patient care? This article is free to 1-Year Classic and 2-Year Premium subscribers.
Strategies and actions to improve clinician experiences. Work/life balance is something nurses are constantly trying to achieve, and many nurses are falling short of that goal. What solutions are your peers using to combat burnout, achieve better nurse work/life balance, and improve patient care? This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Your referral partners increasingly expect robust communications to make patient transfers as seamless as possible, for both the patient and providers. They will have to make a choice. Ultimately, they will look for relationships with organizations that are easy to work with and that can deliver proven quality care. We provide insights and strategies from high-performing organizations. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Your referral partners increasingly expect robust communications to make patient transfers as seamless as possible, for both the patient and providers. They will have to make a choice. Ultimately, they will look for relationships with organizations that are easy to work with and that can deliver proven quality care. We provide insights and strategies from high-performing organizations. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 In this new normal, it’s important to understand how your referral sources work, what they are sending to you versus the competition, how to deepen relationships with these sources, and what differentiates you as a provider in the marketplace. This article is free to 1-Year Classic and 2-Year Premium subscribers.
In this new normal, it’s important to understand how your referral sources work, what they are sending to you versus the competition, how to deepen relationships with these sources, and what differentiates you as a provider in the marketplace. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 Recent research discusses the missed opportunities for discussions about end-of-life, including advance care planning, palliative care, discontinuation of disease-directed treatment, hospice care, and after-death wishes, with outpatients with advanced cancer. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Recent research discusses the missed opportunities for discussions about end-of-life, including advance care planning, palliative care, discontinuation of disease-directed treatment, hospice care, and after-death wishes, with outpatients with advanced cancer. This article is free to 1-Year Classic and 2-Year Premium subscribers.