-
 CMS has released proposed policy changes for 2021 Medicare payment rates under its annual Physician Fee Schedule. Telehealth codes allow physicians to bill for home visits and care planning. We dive into the codes and what they mean. This article is free to 1-Year Classic and 2-Year Premium subscribers.
CMS has released proposed policy changes for 2021 Medicare payment rates under its annual Physician Fee Schedule. Telehealth codes allow physicians to bill for home visits and care planning. We dive into the codes and what they mean. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 TANDEM365 is a complex medical case management program coupled with a robust community paramedicine program that offers rapid response and in-home intervention capabilities. Blending population health management with community paramedicine, the goal of TANDEM365 is to connect all providers across the healthcare continuum to effectively coordinate care and prevent gaps. This article is free to 1-Year Classic and 2-Year Premium subscribers.
TANDEM365 is a complex medical case management program coupled with a robust community paramedicine program that offers rapid response and in-home intervention capabilities. Blending population health management with community paramedicine, the goal of TANDEM365 is to connect all providers across the healthcare continuum to effectively coordinate care and prevent gaps. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
Out of stock

Post-Acute Redefined: Building Integrated, Future-Focused, Post-Acute Solutions
MARCH 5-7, 2020 Loews Coronado Bay Resort, Coronado, California
Purchase a spouse ticket to the Thursday, March 5, Welcome Reception for $35
Premium subscribers receive a 10% discount. Click here to learn about the benefits of a premium subscription. Registering more than 2 spouses? Pay for all your spouses here, provide us with registration information on the first two, and we will follow up with you to obtain registration information on the others. -
 A unified value-based incentive program for post-acute care providers is recommended with a possible 5% withhold. Med-PAC is building on their previous work of the unified prospective payment system across four post-acute settings. This article is free to 1-Year Classic and 2-Year Premium subscribers.
A unified value-based incentive program for post-acute care providers is recommended with a possible 5% withhold. Med-PAC is building on their previous work of the unified prospective payment system across four post-acute settings. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
 A recent study suggests health coaches could provide significant cost savings to patients and health systems, reduce patient hospitalizations and emergency department visits, improve patient health, and improve the quality of care for high-risk patient populations. This article is free to 1-Year Classic and 2-Year Premium subscribers.
A recent study suggests health coaches could provide significant cost savings to patients and health systems, reduce patient hospitalizations and emergency department visits, improve patient health, and improve the quality of care for high-risk patient populations. This article is free to 1-Year Classic and 2-Year Premium subscribers. -
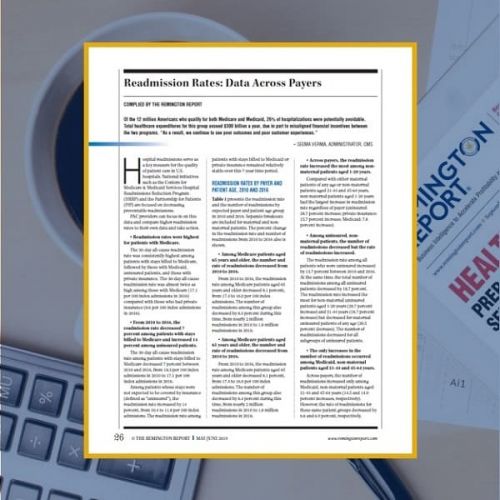 Of the 12 million Americans who qualify for both Medicare and Medicaid, 26% of hospitalizations were potentially avoidable. Total healthcare expenditures for this group exceed $300 billion a year, due in part to misaligned financial incentives between the two programs. This article is free to 1-Year Classic and 2-Year Premium subscribers.
Of the 12 million Americans who qualify for both Medicare and Medicaid, 26% of hospitalizations were potentially avoidable. Total healthcare expenditures for this group exceed $300 billion a year, due in part to misaligned financial incentives between the two programs. This article is free to 1-Year Classic and 2-Year Premium subscribers.